On This Page
Summarise this article using AI
Nimba (Azadirachta indica) – The Village Pharmacy with a Thousand Problems and One Solution
Nimba, the fast-growing, evergreen, popular tree, is botanically known as Azadirachta indica and belongs to the Meliaceae family. Neem is regarded as the tree for solving global problems by the UN National Academy of Sciences in 1992. Nimba is regarded as a village dispensary or pharmacy, as it helps to relieve various diseases.
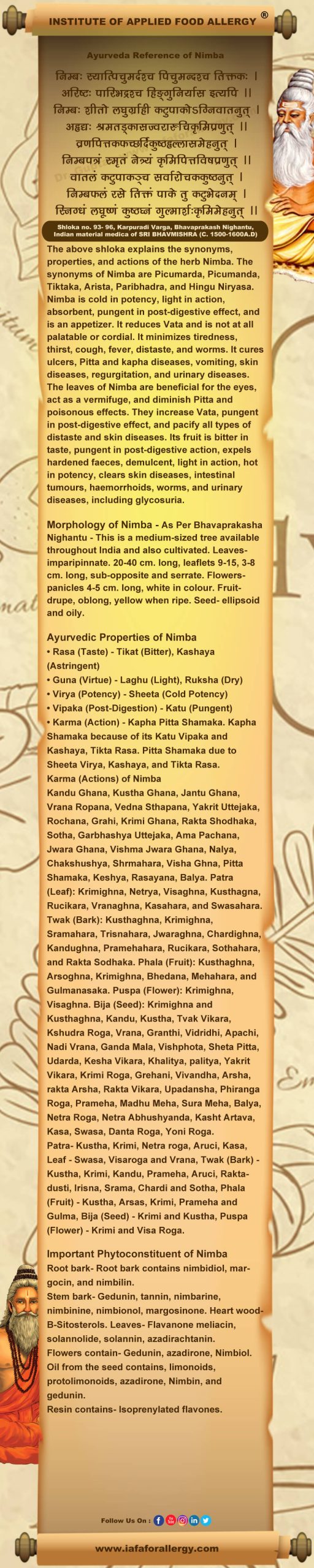
In Ayurvedic classical texts, Nimba is known as Arishta, which means reliever of sickness. Nimba is cold in potency, light in action, absorbent, pungent in post-digestive effect, and is an appetizer. It reduces Vata and is not at all palatable or cordial. It minimizes tiredness, thirst, cough, fever, distaste, and worms.
It cures ulcers, Pitta and kapha diseases, vomiting, skin diseases, regurgitation, and urinary diseases. The leaves of Nimba are beneficial for the eyes, act as a vermifuge, and diminish Pitta and poisonous effects. They increase Vata, pungent in post-digestive effect, and pacify all types of distaste and skin diseases. Its fruit is bitter in taste, pungent in post-digestive action, expels hardened faeces, demulcent, light in action, hot in potency, clears skin diseases, intestinal tumours, haemorrhoids, worms, and urinary diseases, including glycosuria.
Recent research revealed that Neem consists of various secondary metabolites like Gedunin, tannin, nimbarine, nimbinine, nimbionol, and margosinone. Heart wood-B-Sitosterols, flavanone meliacin, solannolide, solannin, azadirachtanin, gedunin, azadirone, Nimbiol. Oil from the seed contains, limonoids, protolimonoids, azadirone, Nimbin, and gedunin, due to which it exhibits various pharmacological activities like anti-allergic, antioxidant, anti-hypertensive, anti-viral, anti-COVID activity, etc.
Basonym of Nimba
निम्बति सिञ्चति स्वास्थ्यमिति, स्वस्थवृत्तिकरमिति यावत् |
Nimba (Azadirachta indica) is a very useful drug which maintains health.
Synonyms of Nimba
According to Morphology
हिंगु निर्यास: – हिंगु इव निर्यासो अस्य ।
The exudate from Nimba resembles Hingu Niryasa (Gum of Ferula Narthex).
According to Properties and Actions
अरिष्ट: – न रिष्टमशुभमस्मात्, सर्वरोगनाशक इत्यर्थ: |
Nimba cures many diseases, and is always good if used.
कृमिघ्न – कृमीन् हन्ति इति |
Nimba is very efficacious in helminthiasis.
नियमन– नियच्छति शमयति रोगानिति |
Nimba alleviates many diseases.
पारिभद्र –परितः भद्रः: कल्याणकर: |
If used, Nimba always does good.
पिचुमर्द: –पिचुं कुष्ठ मर्दयति नाशयतीति |
Nimba is a very efficacious drug when it comes to skin diseases.
सुतिक्तकः – अतितिक्तक: तिक्त द्रव्येषु अग्र गण्य: |
Nimba is one of the best among drugs having bitter taste.
वर त्वच: – वरा श्रेष्ठा त्वक स्येति |
Regional Names of Nimba
- Azad Darakhtul Hind (Arabic)
- Neem tree, Margosa tree (English)
- Nim (Hindi)
- Bevina Mara (Kannada)
- Veppu (Malayalam)
- Kadu Nimba (Marathi)
- Nim (Bengali)
- Nibarh (Punjabi)
- Vembu, Vempu (Tamil)
- Vepa Chettu (Telegu)
- Limarho, Limado (Gujrati)
- Lodho (Oriya)
- Nimu (Siddha)
- Azad Darakhte Hindi (Persian)
Botanical Name of Nimba
Azadirachta indica Juss.
The word Azadirachta is the Persian name meaning the best tree.
Indica is a native of India.
Family – Meliaceae (Nimba Kula)
Ayurveda Reference for Nimba (Azadirachta indica Juss.)
Scientific Classification of Nimba
| Kingdom | Plantae |
| Class | Dicotyledonae |
| Sub-Class | Polypetalous |
| Series | Disciflorae |
| Order | Geraniales |
| Family | Meliaceae |
| Genus | Azadirachta |
| Species | indica |
Classification of Nimba – As Per Charaka and Sushruta
Charaka: Kandughna Mahakshaya
Sushruta: Aragvadhadi Gana, Guduchyadi gana, Lakshadi Gana.
Nimba’s Description in Brihtrayi
| Charaka | Shusruta | Vagbhata (Ashtang Hridya) |
| C. S. Su. 2/ 6 | S. S. Su. 5/ 17 | A. H. Su. 5/ 60 |
| C. S. Su. 3/ 2, 7 | S. S. Su. 36/ 17 | A. H. Su. 10/ 28 |
| C. S. Su. 4/ 14 | S. S. Su. 38/ 5, 49, 63 | A. H. Su. 15/ 1, 6, 17 |
| C. S. Su. 23/ 9, 11, 13 | S. S. Su. 43/ 2, 6 | A. H. Su. 29/ 26, 76 |
| C. S. Su. 27/ 95 | S. S. Su. 45/ 115 | A. H. Sa. 1/ 61 |
| C. S. Vi. 8/ 150, 158 | S. S. Su. 46/ 270, 284, 371 | A. H. Chi. 1/ 7, 49, 65, 66, 75, 119, 162, 163 |
| C. S. Sa. 8/ 54 | S. S. Chi. 1/ 66, 120 | A. H. Chi. 2/ 27 |
| C. S. Chi. 3/ 202, 205, 225, 258, 307 | S. S. Chi. 2/ 89 | A. H. Chi. 3/ 44, 136 |
| C. S. Chi. 4/ 38 | S. S. Chi, 6/ 8 | A. H. Chi. 4/ 21 |
| C. S. Chi. 5/ 115 | S. S. Chi. 8/ 41 | A. H. Chi. 5/ 52 |
| C. S. Chi. 6/ 30, 31, 38 | S. S. Chi. 9/ 5, 7, 14, 38, 48, 51 | A. H. Chi. 6/ 17, 72, 74 |
| C. S. Chi. 7/ 43, 47, 57, 65, 68, 82, 97, 100, 101, 103, 112, 129, 135, 136, 140, 157, 158 | S. S. Chi. 10/ 4, 9 | A. H. Chi. 8/ 23, 103 |
| C. S. Chi. 10/ 32 | S. S. Chi. 11/ 7, 8 | A. H. Chi. 10/ 34, 43, 56 |
| C. S. Chi. 12/ 62, 71 | S. S. Chi. 17/ 21, 23, 24, 43 | A. H. Chi. 12/ 8 |
| C. S. Chi. 14/ 56, 187, 215 | S. S. Chi. 18/ 47, 51 | A. H. Chi. 13/ 11, 35 |
| C. S. Chi. 15. 126, 136, 139, 182, 190 | S. S. Chi. 19/ 42 | A. H. Chi. 16/ 13, 23, 39, 43 |
| C. S. Chi. 16/ 48, 53, 63, 87, 122 | S. S. Chi. 20/ 21, 27, 28, 38, 39, 55 | A. H. Chi. 17/ 25 |
| C. S. Chi. 17/ 97 | S. S. Chi. 22/ 25, 47 | A. H. Chi. 18/ 2, 5, 7 |
| C. S. Chi. 20/ 34, 35 | S. S. Chi. 23/ 15 | A. H. Chi. 19/ 2, 9, 11, 18, 26, 33, 36, 37, 38, 39, 41, 50, 61, 65, 79, 91 |
| C. S. Chi. 21/ 50, 53 | S. S. Chi. 24/ 6 | A. H. Chi. 21/ 52, 58 |
| C. S. Chi. 23/ 51, 69, 79, 202, 241 | S. S. Chi. 25/ 23 | A. H. Ka. 1/ 17 |
| C. S. Chi. 25/ 82, 83, 93 | S. S. Chi. 37/ 33 | A. H. Ka. 4/ 23 |
| C. S. Chi. 26/ 237 | S. S. Chi. 38/ 59 | A. H. U. 2/ 13 |
| C. S. Chi. 27/ 27, 51 | S. S. Ka. 8/ 136 | A. H. U. 3/ 44, 48, 55 |
| C. S. Chi. 29/ 148 | S. S. Sa. 10/ 23 | A. H. U. 5/ 11, 20, 37, 39 |
| C. S. Chi. 30/ 73, 82, 98, 253, 258, 279 | S. S. U. 12/ 13 | A. H. U. 9/ 22, 24, 32 |
| C. S. Ka. 2/ 8 | S. S. U. 19/ 15 | A. H. U. 11/ 22 |
| C. S. Si. 3/ 59 | S. S. U. 34/ 6 | A. H. U. 13/ 6 |
| C. S. Si. 4/ 18 | S. S. U. 39/ 138, 184, 186, 209, 219, 246, 257, 264, 277 | A. H. U. 16/ 17, 39 |
| C. S. Si. 8/ 7 | S. S. U. 43/ 17 | A. H. U. 18. 50 |
| S. S. U. 48/ 19 | A. H. U. 22/ 38, 50, 52, 55, 56, 68, 78, 106 | |
| S. S. U. 57/ 8, 9 | A. H. U. 24/ 17, 21, 22, 34 | |
| S. S. U. 61/ 23 | A. H. U. 25/ 42, 43, 55, 67 | |
| S. S. U. 64/ 33 | A. H. U. 32/ 4, 13 | |
| S. S. U. 65/ 9 |
Nimba’s Description in Brihtrayi as Arishta
| Charaka | Shusruta | Vagbhata (Ashtang Hridya) |
| C. S. Chi. 3/ 240, 257 | S. S. Su. 19/ 28 | A. H. Su. 6/ 75 |
| C. S. Chi. 7/ 151 | S. S. Su. 39/ 3 | A. H. Su. 15/ 16 |
| S. S. Su. 44/ 6 | A. H. Chi. 5/ 28 | |
| S. S. Su. 46/ 197, 262 | A. H. Chi. 12/ 1, 18 | |
| S. S. Chi. 9/ 28, 46, 50 | A. H. U. 14/ 14 | |
| S. S. Chi. 16/ 17 | A. H. U. 30/ 34 | |
| S. S. Chi. 25/ 43 | ||
| S. S. U. 39/ 222 | ||
| S. S. U. 41/ 50 |
Nimba’s Description in Brihtrayi as Kaidarya / Kaitarya
This has been variously interpreted to be Maha Nimba, Katphala, and Puti Karanja. Katphala may be a suitable substitute, but it can not be classed among the Nimba varieties. Ailanthus excelsa or Murraya koenigii can be the only possibilities. The Nimba Bheda called Dreka or Bakaina has been described as different by the Nighnatus.
Charaka Samhita: C. S. Su. 4/ 9, 48, C. S. Vi. 7/ 17, C. S. Chi. 10/ 25, 35, C. S. Chi. 26/ 54
Sushruta Samhita: S. S. Chi. 18/ 22, S. S. Sa. 10/ 69, S. S. U. 28/ 4
Ashtanga Hridya: A. H. U. 1/ 48
Nimba’s Description in Brihtrayi as Tiktottama
It may be either Patola or Nimba.
Ashtanga Hridya: A. H. Ka. 1/ 24
Nimba’s Description in Brihtrayi as Paribhadraka, Paribhadra
Paribhadra and Parijata appear to be synonyms and may be identified with species of Erythrina such as E. tuberosa Roxb., and E. indica Lam., etc. Its description by Dalhana as a tree having red flowers and spines, and called Kantakipalasa or Pharahada, justifies the above suggestion. The use of Nimba- and Harasimgara (Nyctanthes arbor-tristis Linn.) may be due to their being substituted in its place. It may be noted that its bark is being used in place of Rohitaka bark, probably due to its action in liver complaints.
Sushruta Samhita: S. S. Su. 11/ 11, S. S. Su. 29/ 64, S. S. Chi. 4/ 32, S. S. Ka. 3/ 9, S. S. Ka. 6/ 3, S. S. U. 32/ 3, S. S. U. 54/ 26, S. S. U. 58/ 48
Ashtanga Hridya: A. H. Su. 30/ 8, A. H. Chi. 11/ 14, A. H. Chi. 20/ 26A. H. U. 2/ 59, A. H. U. 3/ 45
Nimba’s Description in Brihtrayi as Pichu Marda
Charaka Samhita: C. S. Vi. 7/ 17, C. S. Vi. 8/ 143, C. S. Chi. 3/ 252, C. S. Chi. 7/ 46/ 131, 144, C. S. Chi. 21/ 51, 58, 97, C. S. Chi. 25/ 88, C. S. Chi. 27/ 49, C. S. Ka. 1/ 25
Sushruta Samhita: S. S. Chi. 9/ 7, 8, 9, S. S. Chi. 20/ 15, S. S. Chi. 22/ 54, S. S. Chi. 31/ 5, S. S. Ka. 6/ 3
Ashtanga Hridya: A. H. Chi. 1/ 89, A. H. Chi. 6/ 49, A. H. U. 37/ 83
Historical Background of Nimba
In the Vedic literature, Nimba is delineated several times. But its stem is not recommended for rituals, but it is used as a toothbrush. Charaka delineated Nimba under Kandughna drugs (anti-pruritic drugs). Kaidarya mentioned that among the Sangya Sthapana dravyas, Parvata Nimba is considered to be Parvata Nimba according to Cakrapani. Caraka used the flowers of Nimba for Sirovirecana (Nasya).
He indicated it for external use in skin diseases also. Susruta prescribed it in Mutraghata (Urinary obstruction) treatment along with other plants. Vagbhata described its seed oil as very effective in the treatment of grey hair and hair fall as nasal drops for one month (with milk). It is also quoted as a Vamana dravya (emetic) by Caraka, etc. Among Pancha Tiktas (five bitters), Nimba mula Tvak (root bark of Neem) is mentioned.रसात में ये सर्वत्र देखा जाता है | इसका वर्षायु, प्रसरी, मांसल एवं चिकना क्षुप होता है |ये भारत में सर्वत्र पाया जाता है |
External Morphology of Azadirachta indica Juss.
Habit: Nimba is a large, shady tree, up to 25 meters tall.
Bark: Bark of the Nimba tree is grey, cracked, and rough on mature branches.
Leaves: Leaves up to 30 cm. long, leaflets of Nimba are 5-13 or 12-16, obliquely lanceolate, 3-7 × 1-3 cm., cuneate at base, dentate at margins, crenate-serrate, oblique, up to 6 × 2 cm.
Inflorescence: Nimba has axillary panicles, an inflorescence up to 30 cm long, with long peduncles. Flowers white, Corolla 10 mm. across; flowers 2 2-merous, often up to 8-merous. Calyx 5-fid, lobes ovate. Petals oblanceolate, Ca 5 mm. Staminal tuber dilated above, 10-fid at tip, anthers exerted. Ovary globose 3-locular, style elongate, stigma 3 3-lobed, with a basal rim.
Fruits: Fruits of Nimba are drupaceous, baccate, 1-seeded, pulpy, green when young, yellow when ripe, drupe globose, pulpy white with a very large exarillate seed. Drupes (fruit) ovoid, oblong.
Flowering and Fruiting Time of Nimba
Plant flowers from February to April, and they bear fruit in April-June. Flowering and fruiting occur during the spring to summer season.
Distribution of Nimba
The plant is commonly found throughout India and especially in drier and warmer regions of north-western and central India. It is very common, planted in gardens, along the roadside, in house premises, and it also occurs as a self-grown plant. Trees are found in both states, cultivated or planted, as well as wild or natural. It is popularly planted as a shade tree, purifying the atmosphere at various places. Plants are wild in dry and warm forest regions.
The Useful Part of Nimba
Patra (Leaf), Twak (Bark), Bija (Seed), Phala (Fruit), Puspa (Flowers), and Niryasa (Resin).
Leaf – Pinnately branched leaves with ovate lanceolate, subfalcate, and bluntly serrate leaflets having an acute apex, measuring up to 5 cm in length and 1.5 cm in breadth. The leaves are up to 50 cm long, clustered at the end of the branches, which also bear bunches of lilac flowers in terminal panicles. Leaflets, when fresh, are bright green but turn greyish on drying. Has got a disagreeable odor. The taste is very bitter.
Bark – Bark is channeled or quilled pieces of tough and fibrous bark ranging from 3 mm to 10 mm in thickness. The outer surface is greyish brown to black in color, rough, scaly, and irregularly fissured, especially in the bark obtained from older stems. The inner surface is cream in color, conspicuously laminated, and coarsely fibrous. The transversely cut portion shows a smooth, minutely chequered surface. On breaking, it becomes fibrous and has a bitter and astringent taste.
Varieties of Nimba
There are three varieties of Nimba we come across in various contexts in the Ayurvedic literature:-
- Aakasha Nimba – Millingtonia hortensis
- Nimba – Azadirachta indica
- Maha Nimba – Melia azederach
- Parvat Nimba – Ailanthus exelsa (Aralu)
Important Phytoconstituent of Nimba
Bark contains nimbine or margosine, a resinous principle, nimbidine, nimbine 0.03, nimbosterol, a volatile oil, and tannin 6%. Flowers also yield a volatile oil. Leaves contain bitter substances in lesser quantity but are more soluble in water in comparison to the solubility of bark bitter substances. Taddy or sap contains bitter substances, glucose, colouring matter, gum protides, and ash. Ash contains potassium, iron, aluminium, calcium, and carbon dioxide. Seeds yield fixed oil up to 40 per cent, which is known as margosa oil. Margosa oil contains bitter substances, oleic acid 49- 61 %, linoleic acid 2- 1/5 %, palmitic acid 12- 15 %, stearic acid 14- 23 % etc., and nimbosterol and other contents.
Leaves – Leaves contain Nimbin, Nimbinene, Nimbandiol, Nimbolide, Quercitin, B-sitosterol, Azadirone, Azadiradione, and Azadirachtin.
Bark – Bark has Nimbin, Nimbinin, Nimbidin, Margolone, and Margolonone. Seeds contain Nimbin, Nimbidin, Azadirachtin, Chlorogenic acid, Salanin, and 4-Epinimbin.
Flower – Flowers possess Nimbosterol, Myricitin, and Kaempferol.
Fruits – Fruits of Nimba yielded gedunin, Azadiradione, Azadirone, and Deacetyl Azadirachtinol.
Recent Research on Nimba (Azadirachta indica)
Anti-Fertility Activity –
- Neem oil has been reported to possess strong spermicidal action against rhesus monkey and human spermatozoa within 30 seconds of mixing with semen. (Sinha et al, 1984).
- The lethal concentration for humans, spermatozoa was 1000 mg and 250 mg per 100 in 5 and 30 minutes, respectively. (Sharma & Saxena, 1959).
- An injection of neem oil (1001) into the uterine horn created an immunological response and prevented pregnancy for five months. (Upadhyay et al, 1990)
Anti-Inflammatory & Anti-Arthritic Activity –
- Nimbidin (40 mg/ kg body weight) significantly reduced acute paw edema in rats induced by phlogistic agents, carrageenin, and kaolin. Its action is compared to phenytoin (100 mg/ kg). (Pillai & Santha Kumar. 1981).
- Bark extract produced significant anti-inflammatory activity. (Tidjani et al; 1989, Lorenz, 1976 & Kakai, 1976).
Cardiovascular Activity – Extract of neem leaves showed profound hypotension and a minimal negative chronotropic effect. It also exhibited a weak antiarrhythmic activity in rabbits against oculain-induced dysrhythmia. (Thompson & Anderson, 1978).
Anti-Diabetic Activity –
- Aqueous extract of leaves decreased the blood sugar levels in dogs (on i.v. admn.) and prevented adrenaline as well as glucose hyperglycaemia. The onset of action was at 30 min- 4 hours. (Murthy et al, 1958).
- Neem oil does not produce hypoglycemia in normal animals, but it does improve glucose tolerance in partially pancreatectomised dogs. The hypoglycemic effect is about 24.77 % to 26.38 % in five hours (Pillai & Santha Kumari, 1981).
Skin Disorders & Anti-Microbial Activity –
- It is found to be effective in case of acute eczema, ringworm infestation, and scabies (Singh et al, 1978).
- The antimicrobial activity of different neem extracts and neem products is well documented. (Shankara Narayanan, 1965; Rao et al, 1986; Singh et al, 1988; Patel & Trivedi, 1962).
CNS Activity –
Leaf extract showed varying degrees of CNS depressant activity in mice. (Singh et al; 1987; Singh et al; 1980)
Immunostimulant Activity –
- The aqueous extract of bark showed anti-complementary activity, acting both on alternative and classical pathway activation (Vander et al, 1987 & 1989).
- The aqueous extract of the leaf possessed potent immunostimulant activity as evidenced by both humoral and cell-mediated responses (Sen et al, 1992).
- Kumar, Sanjay & Vandana, Udaya & Agrawal, divya & Hansa, Jagadish. (2015). Analgesic, Anti-inflammatory, and Anti-Pyretic Effects of Azadirachta indica (Neem) Leaf Extract in Albino Rats. International Journal of Science and Research (IJSR). 4. 713- 721. Neem (Azadirachta indica), popularly known as ‘Wonder tree’, is an evergreen tropical tree, which has been reported to have beneficial effects on various disease pathologies from ancient times. Such health benefits are the sum of molecular actions of the natural ingredients present in it. Among all ingredients, azadirachtin, nimbidin, flavonoids, and triterpenoids are notable for their beneficial effects against disease pathology. Neem has been reported to have anti-allergenic, anti-dermatic, anti-feedant, anti-fungal, anti-inflammatory, anti-pyorrhoeic, and anti-scabic modes of action. Besides these, neem is also beneficial for cardiac, diuretic, insecticidal, larvicidal, nematicidal, spermicidal, and other biological activities. Though here in the present study, our focus was only on three parameters, i.e., whether neem leaf extracts (NLE) can contribute to anti-analgesic, anti-inflammatory, and antipyretic action in albino rats, which is a novel one. Our experimental observations revealed that NLE has analgesic, anti-inflammatory, and antipyretic effects in Albino rats.
- Baghel, Shalu & Singh, Charanjeet. (2019). ANTIHYPERLIPIDEMIC ACTIVITY OF METHANOLIC EXTRACT OF AZADIRACHTA INDICA. Journal of Biomedical and Pharmaceutical Research. 8. 10. 32553/ jbpr. v8i6. 678. Hyperlipidemia often results from delayed or defective clearance or overproduction of VLDL by the liver, which is subsequently transformed into LDL. The whole plant of Azadirachta indica was collected from the local areas of the Jaipur district of Rajasthan. The plant is authenticated by the University of Rajasthan by Dr. Manju Sharma, dept of Botany. Selected medicinal plants were cut into small pieces, cleaned, and shade-dried at room temperature, then subjected to physical evaluation with different parameters. Macerated 5 g of air-dried drug coarsely powdered with 100 ml of ethanol of the specified strength in a closed flask for twenty-four hours, shaking frequently during six hours, and allowed to stand for 18 h. About 2-3 g of powder is accurately weighed in a china dish and kept in a hot air oven maintained at 110±1 °C for four hours. After cooling in a desiccator, the loss in weight was recorded. This procedure was repeated till a constant weight was obtained. For insoluble ash value, boil the ash for 5- 10 minutes with 25 ml of diluted hydrochloric acid, collect the insoluble matter in a Gooch crucible, wash with hot water, ignite, and weigh. The whole plant of Azadirachta indica was reduced to fine powder and was subjected to maceration in a 1-liter conical flask for 7 days at room temperature with alcohol (70 %) and water (30 %). In the present study, we aimed to screen various extracts of selected plants on the cholesterol-induced hyperlipidemic rat model. Thus, the results of the present investigation clearly indicated that the selected medicinal plants possess good antihyperlipidemic activity in atherogenic diet-induced hyperlipidemic rats and led to the development of a new Herbal formulation possessing antihyperlipidemic and antiatherosclerotic activities. This is the first study that investigates hypolipidemic activity.
- SALAZAR, Daniel & Hoyos, Rodrigo & Orozco-Sánchez, Fernando & Arango, Myrtha & Gomez Londoño, Luisa. (2015). Antifungal activity of neem (Azadirachta indica: Meliaceae) extracts against dermatophytes. Acta Biológica Colombiana. 20. 201- 207. 10. 15446/ abc. v20n3. 45225. To assess the antifungal activity of methanolic extracts from neem tree (Azadirachta indica A. Juss.), several bioassays were conducted following the M38-A2 broth microdilution method on 14 isolates of the dermatophytes Trichophyton mentagrophytes, Trichophyton rubrum, Microsporum canis, and Epidermophyton floccosum. Neem extracts were obtained through methanol-hexane partitioning of mature green leaves and seed oil. Furthermore, high-performance liquid chromatography (HPLC) analyses were carried out to relate the chemical profile to their content of terpenoids, widely known for their antifungal activity. The antimycotic Terbinafine served as a positive control. Results showed that there was total growth inhibition of the dermatophytes isolates at minimal inhibitory concentrations (MIC) between 50 μg/ mL and 200 μg/ mL for leaf extract, and between 625 μg/ mL and 2500 μg/ mL for seed oil extract. The MIC of positive control (Terbinafine) ranged between 0.0019 μg/ mL and 0.0313 μg/ mL. Both neem leaves and seed oil methanol extracts exhibited different chromatographic profiles by HPLC, which could explain the differences observed in their antifungal activity. This analysis revealed the possible presence of terpenoids in both extracts, which are known to have biological activity. The results of this research are a new report on the therapeutic potential of neem for the control of dermatophytosis.
- Mostofa, Mahbub & Choudhury, Mohammed & Hossain, Md.Monir & Islam, Md & Islam, Muh & Sumon, Md Mahmudul Hasan. (2008). Antidiabetic effects of Catharanthus roseus, Azadirachta indica, Allium sativum, and glimepiride in experimentally diabetic induced rats. Bangladesh Journal of Veterinary Medicine. 5. 10. 3329/ bjvm. v5i1.1324. Catharanthus roseus (Nyantara), Azadirachta indica (Neem), and Allium sativum (Garlic) are medicinal plants used in Ayurveda for treating various diseases, one of which is diabetes mellitus. In the present study of 12 12-month period from January to December 2007, aqueous extract of these plants was prepared, and the blood glucose-lowering effect and improvement of body weight gain in Streptozotocin (50 mg/ kg bwt i.p.) induced diabetic rats were measured and compared with that of the patent drug glimepride in the Department of Pharmacology, Bangladesh Agricultural University, Mymensingh. Rats were administered Catharanthus roseus, Azadirachta indica, and Allium sativum extracts at the dose rates of 1g/ kg, 500 mg/ kg, and 1g/ kg bwt orally for 14 days, respectively. Blood glucose level and body weight were measured by the Glucotrend kit and electronic balance, and compared with a patent drug, Glimepride, at a dose rate of 100 mg/ kg bwt. The data were compared statistically by using Student’s unpaired t-test. The herbal preparations of these plants significantly increased body weight gain and decreased blood glucose as compared with the patent drug. The present study clearly indicated the significant antidiabetic activity of Catharanthus Roseus, Azadirachta indica, and Allium sativum and supports the traditional usage of the herbal preparations by Ayurvedic physicians for the therapy of diabetics.
- Santra, Soumya & Naik, M.R. & Behera, R. & Agrawal, Divya & Kumar, Sanjay & Patnaik, S. (2014). Antipyretic effect of Azadirachta indica leaf extract (Neem Leaf Extract) on albino rats. Research Journal of Pharmaceutical, Biological and Chemical Sciences. 5. 669- 673. Evaluation of antipyretic activity of Neem Leaf Extract (NLE) by using Brewer’s yeast-induced pyrexia model. In this study, the albino rats were randomly divided into groups of six, each consisting of 6 rats. Group I: Control (distilled water 0.5 ml/ rat); Group II: Standard (Paracetamol 100 mg/ kg intraperitoneally); Group III, IV, V, VI (NLE 62.5, 125, 250, 500 mg/ kg body weight intraperitoneally, respectively). It is a randomized controlled experimental study. Fever was induced by injecting 20 ml/ kg body weight of 20 % suspension of brewer’s yeast subcutaneously below the nape of the neck. Those animals that had a constant rectal temperature or a variation of less than 1°C were included in the study. Drugs were given after the development of pyrexia, and temperatures were recorded. Paracetamol at 100 mg/ kg orally was taken as the standard drug. NLE 62.5 mg/ kg body weight showed no significant fall in temperature, whereas NLE 125 mg/ kg body weight decreased the temperature significantly from the 4th hour of its injection, along with NLE 250 mg and 500 mg/ kg body weight. NLE caused a significant fall in temperature from the 1st hour onwards. Distilled water did not show any antipyretic effect on Yeast-induced pyrexia. Thus, NLE exhibited significant (p< 0.05) antipyretic activity with the progressive increase in dose.
- Raut, Ranjit R., & Sawant, Ajit, & Jamge, Bhagyshree. (2014). Antimicrobial activity of Azadirachta indica (Neem) against Pathogenic Microorganisms. Journal of Academia and Industrial Research. 3. 327- 329. Plants have been a source of herbal remedies throughout the history of mankind. Various medicinal plants have been used for years in daily life to treat diseases all over the world. In the present study, antimicrobial activity of Azadirachta indica was evaluated against Gram-negative pathogenic bacteria (Escherichia coli, Salmonella typhi, and Vibrio cholerae) and Gram-positive bacteria (Bacillus subtilis). Azadirachta indica leaves and barks were collected from the fields of Botanical Garden in Padmashri Vikhe Patil College, Pravaranagar, and pure cultures of the test organisms used for antimicrobial study were obtained from the Department of Microbiology, Pravara Institute of Medical Sciences, Loni. All the test organisms were screened for their antibacterial activity against the leaf and bark extract of A. indica by the agar well diffusion method. Leaf and bark extract of Azadirachta indica showed more inhibition zone against Vibrio cholerae and Bacillus subtilis, while E. coli and S. typhi are less susceptible to neem extract.
- Adamu, Muhammad & Lawan, Ibrahim & Abubakar, Ahmed & Dangora, Ibrahim. (2019). Antimicrobial Activity of Azadirachta indica (Neem) Leaf Extract Against Some Clinical Isolates. The present study was carried out at the Microbiology and Chemistry Laboratories, Federal University Dutse, Jigawa State. To investigate the activity of neem leaf extract against some clinical isolates. The test organism includes Escherichia coli, Klebsiella pneumoniae, and Staphylococcus aureus. The phytochemical compounds present in the neem were extracted using ethanol as a solvent. The Soxhlet extractor was used to get the extract. Phytochemical screening was carried out using the standard methods. Some of the examined phytochemicals are Alkaloids, saponins, phenols, Tannins, and Flavonoids. The extract is more effective against Gram-negative E. coli and K. pneumoniae as compared to S. aureus, a Gram-positive bacterium. The zone of inhibition of the extract at 125 mg/ ml is 21 and 14. For Gram-negative and Gram-positive bacteria, respectively. The mean of the minimum inhibitory concentration of A. indica leaf extract, the minimum inhibitory concentration (MIC) of the extract in vitro revealed to be at much lower concentration 50mg/ml against E. coli as compared to 100mg/ml against S. aureus the minimum bactericidal concentration (MBC) of A. indica leaf extract shows that the extract have a bacteriostatic effect against gram negative bacteria with static effect against gram positive bacteria.
- Prabagar, Subramaniam & Nandakumar, Jeyarani & Prabagar, Jasotha & Thuraisingam, Suganja. (2020). SPC Journal of Plant Sciences Antimicrobial activity of Azadirachta Indica (neem) leaves and stem bark aqueous extracts. Background: Azadirachta indica is a multipurpose tree called Neem, which is used in Ayurvedic medicine for skin infections and as a household pesticide. Methods: Aqueous extraction of plant material, such as leaf and stem bark, was investigated for anti-microbial activity without altering concentration. Results: The Results of the study revealed that all extracts had inhibitory activity against Staphylococcus aureus with a clear zone of 2.6 cm, which is higher than the streptomycin control. The inhibition zone was found in descending order against Klebsiella, Pseudomonas, and Bacillus species. Antifungal activity of bark extract of Azadirachta indica against Aspergillus and Yeast showed the inhibitory growth of 64.2 % and 64 % whereas the leaf extract showed less inhibition than the bark extract. Conclusion: The findings reveal that bark and leaf aqueous extracts have wide-ranging activity.
- Patil, Prabhakar & Patil, Sudha & Mane, Abhay & Verma, Sushilkumar. (2013). Antidiabetic activity of alcoholic extract of Neem Azadirachta Indica root bark. National Journal of Physiology, Pharmacy and Pharmacology. 3. 142- 146. 10. 5455/ njppp. 2013. 3. 134- 138. Background: Most of the parts of the neem tree were studied in detail by many researchers, but the neem root bark was not screened for antidiabetic effect. To evaluate the antidiabetic effect of neem root bark, this study was conducted. Aims & Objective: The present study was undertaken to evaluate the 70% alcoholic neem root bark extract (NRE) in diabetes. Materials and Methods: Basal blood sugar levels were estimated in overnight fasted Wistar albino rats of either sex. To evaluate the antihyperglycemic action of Neem root bark extract (NRE), an OGTT was done by giving glucose orally 60 minutes after giving the standard drug (Glibenclamide), the Test drug (NRE) in the doses of 200, 400, and 800 mg/ kg, and blood sugar levels were estimated every half hour up to 4 hours. To evaluate hypoglycemic activity in alloxan-induced diabetic rats, similar doses were administered once daily for 15 days. Blood sugar levels were estimated by using a glucometer. Results: For the glucose tolerance test, Glibenclamide showed a significant (p< 0.01) reduction in blood sugar levels. The NRE showed statistically significant results in only the 800 mg/ kg dose. In comparison to glibenclamide, it did not show. In alloxan-induced diabetes, Glibenclamide showed a significant (p< 0.01) reduction in blood sugar levels. The NRE showed statistically significant results in only the 800 mg/ kg dose. Conclusion: Neem root has antihyperglycemic and hypoglycemic activity. It is not as significant as glibenclamide.
- Khan, Shaista. (2015). In Vitro Analysis of Antiallergic Activity of Neem (Azadirachta Indica) for Reduction of Wheat Allergens. Sindh Univ. Res. Jour. (Sci. Ser..). 47. 485- 488. Abstract: Plants are the origin of life on earth and have been essential for people’s livelihood since ancient times. Plants have been an excellent source of medicine. Survival of mankind is unfeasible without the plant kingdom. The name of the Neem tree in Sanskrit is ‘Arishtha’, which means that it is a reliever of ‘Sickness’. According to the healing system of Ayurveda, the Neem tree will strengthen individual resistance to disease, and Neem efficiently regulates the immune system and other functions. Neem is used for a wide range of disorders, including diarrhea, inflammatory diseases, antimicrobials, skin diseases, urinary disorders, antiseptics, bronchitis, cough, asthma, fever, hypertension, and infected burn skin diseases, malaria, and many more ailments. In the present study, characterization of wheat protein has been done, and possible allergens having molecular weights of 7 kDa, 9 kDa, 15 kDa, 12 kDa, 17 kDa, 36 kDa,, 45 kDa, and 77 kDa have been found. But after the treatment of wheat protein with Neem (Azadirachta indica) extract showed a high reduction of allergenic proteins. There are no allergic bands that have been seen after treatment with Neem.
- Mankala, Dr. Santhosh Kumar. (2011). In vivo Antidiabetic evaluation of Neem leaf extract in alloxan-induced rats. Journal of Applied Pharmaceutical Science. 1. 100-105. Azadirachta indica has been used medicinally throughout history by many different cultures. Many compounds have been found in the exudates of the Azadirachta indica plant that have been used medically by humans. We have examined the pharmacological hypoglycemic action of Azadirachta indica in diabetic rats. After treatment for 24 hrs, Azadirachta indica 250 mg/ kg (single dose study) reduced glucose (18 %), cholesterol (15 %), triglycerides (32 %), urea (13 %), creatinine (23 %), and lipids (15 %). Multiple dose study for 15days also reduced creatinine, urea, lipids, triglycerides, and glucose. In a glucose tolerance test in diabetic rats with neem extract 250 mg/kg, glucose levels were significantly less compared to the control group. Azadirachta indica significantly reduces glucose levels on the 15th day in diabetic rats. Azadirachta indica serves as an important alternative source in the management of diabetes mellitus, involved in reducing increased blood glucose during diabetes, which should be examined further by oral hypoglycemic therapy.
- Thiagarajan, Kalaivani & Meignanam, E. & Premkumar, N. & Siva, Ramamoorthy & Vijayakumar, Vijayaparthasarathi & Chandrasekaran, Rajasekaran & Subramanian, Ramya & Jayakumararaj, R. (2009). Studies on Hepatoprotective Properties of Leaf Extracts of Azadirachta indica A. Juss (Meliaceae). Ethnobotanical Leaflets. 13. 165- 170. The present study was carried out to evaluate the hepatoprotective role of leaf extracts of Azadirachta indica A. Juss. Hepatoprotective activities of ethanolic and aqueous extracts of A. indica were examined against carbon tetrachloride-induced liver damage in mice using silymarin as a control. Enzyme activities of Serum Glutamate Oxaloacetate Transaminase (SGOT), Serum Glutamate Pyruvate Transaminase (SGPT), and Alkaline Phosphatase (ALP) were analyzed. Phytochemical leaf extracts of A. indica exhibited significant hepatoprotective activity. Ethanolic and aqueous leaf extracts of A. indica exhibited moderate activity over carbon tetrachloride-treated animals. Results confirm the traditional ethnomedicinal use of A. indica as a potential source of hepatoprotective agents.
- Chattopadhyay, Rabiranjan & Bandyopadhyay, M. (2006). Effect of Azadirachta indica leaf extract on serum lipid profile changes in normal and streptozotocin-induced diabetic rats. African Journal of Biomedical Research. 8. 10. 4314/ ajbr. v8i2. 35769. Effects of Azadirachta indica leaf extract on serum lipid profile changes in normal and streptozotocin-induced diabetic rats have been studied with a view to elucidating its possible effect on cardiovascular disease induced by hyperglycemia. It was observed that A. indica leaf extract significantly reduced the total cholesterol, LDL- and VLDL-cholesterol, triglycerides, and total lipids of serum in streptozotocin-induced diabetic rats, but HDL-cholesterol levels remained unchanged when compared with streptozotocin-induced diabetic control animals. African Journal of Biomedical Research Vol. 8 (2) 2005: 101- 104
- Shahbaz, Benish & Akhtar, Shabana & Muddassir, Maria & Yasmin, Shagufta & Akram, Ayesha & Majeed, Muhammad & Ahmad, Mukhtiar & Shafiq, Muhammad & Arshad, Shafia & Hadi, Faheem & Tahir Maqbool, Dr & Hayat, Sikander & Muhammad, Tahir. (2023). Anti-diabetic activity of a novel Phytoformulation of Tribulus terrestris, Prunus dulcis, Cicer arietinum, and Azadirachta indica in streptozotocin-induced diabetic rats. 19. 360- 373. Background and Objective: Selected medicinal plants have been investigated as an alternative source for the treatment of Streptozotocin (Stz) induced diabetes. The aim of the current study was to assess the anti-diabetic effects of selected plant formulations, Tribulus terrestris, Prunus dulcis, Cicer arietinum, and Azadirachta indica in diabetic rats induced by streptozotocin. Plants included in this phytoformulation have shown antioxidant, anti-diabetic, and anti-inflammatory properties evident in previous research.
- Basha, Saleem & Baruah, Mriganka & Shaker, A. & Kondaveeti, Dr.Suresh & Narayana, S. (2012). Hypoglycemic and hypolipidemic effect of Azadirachta indica seed oil and mehani (polyherbal formulation) on alloxan-induced diabetic albino rats. Research Journal of Pharmaceutical, Biological and Chemical Sciences. 3. 239- 246. The present study aims to investigate the hypoglycaemic and hypolipidemic effect of Azadirachta indica seed oil and Mehani (Poly Herbal Formulation) in alloxan-induced diabetic Wistar albino rats. The rats were divided into 6 groups, each consisting of 6 rats: Control (Normal) rats, diabetic induced rats received alloxan (150/ Kg in 3 doses), diabetic induced rats treated with Azadirachta indica seed oil (5ml/ Kg orally for 21 days), Normal rats treated with Azadirachta indica seed oil, Diabetic induced rats treated with Mehani (2 gm/ 60 Kg orally for 21 days) and Normal rats treated with Mehani. The rats were monitored for plasma glucose, glucose metabolising enzymes, hexokinase and glucose-6-phosphatase, and Lipid profile. Alloxan induced diabetic rats shows a high blood glucose with altered lipid profile and altered level of glucose metabolising enzymes which was counteracted upon treatment with Azadirachta indica seed oil and Mehani which shows significant (p< 0.01) reduction in blood glucose, serum cholesterol, serum triglyceride and glucose- 6- phosphatase level and significant (p< 0.01) increase in the level of hexokinase and serum HDL suggesting its hypoglycaemic and hypolipidemic role. Again, in comparison to Azadirachta indica seed oil, Mehani (Poly Herbal Formulation) has more hypoglycaemic and hypolipidemic effects.
- Satyanarayana, K & Sravanthi, K & Shaker, I., Anand & Ponnulakshmi, R. (2015). Molecular approach to identify antidiabetic potential of Azadirachta indica (neem) on the expression of insulin signaling molecules and glucose oxidation in skeletal muscle of high-fat and fructose-induced type-2 diabetic adult male rat. Journal of Ayurveda and Integrative Medicine. 10. 4103/ 0975- 9476. 157950. Background: Azadirachta indica (Neem) is a medicinal plant, used in Ayurveda for treating various diseases, one of which is diabetes mellitus. It is known to possess anti-inflammatory, antipyretic, antimicrobial, antidiabetic, and diverse pharmacological properties. However, the molecular mechanism underlying the effect of A. indica on insulin signal transduction and glucose homeostasis is obscure. Objective: The aim was to study the effects of A. indica aqueous leaf extract on the expression of insulin signaling molecules and glucose oxidation in the target tissue of high-fat and fructose-induced type-2 diabetic male rats. Materials and methods: The oral effective dose of A. indica leaf extract (400 mg/ kg body weight [b. wt]) was given once daily for 30 days to high-fat diet-induced diabetic rats. At the end of the experimental period, fasting blood glucose, oral glucose tolerance, serum lipid profile, and the levels of insulin signaling molecules, glycogen, and glucose oxidation in the gastrocnemius muscle were assessed. Results: Diabetic rats showed impaired glucose tolerance and impairment in insulin signaling molecules (insulin receptor, insulin receptor substrate- 1, phospho- IRS- 1(Tyr- 632), phospho- IRS- 1(Ser- 636), phospho- Akt (Ser- 473), and glucose transporter 4 [GLUT- 4] proteins), glycogen concentration and glucose oxidation. The treatment with A. indica leaf extract normalized the altered levels of blood glucose, serum insulin, lipid profile, and insulin signaling molecules as well as GLUT-4 proteins at 400 mg/ kg b. wt dose. Conclusion: It is concluded from the present study that A. indica may play a significant role in the management of type-2 diabetes mellitus by improving the insulin signaling molecules and glucose utilization in the skeletal muscle.
- Awah, Francis & Uzoegwu, Peter & Ifeonu, Patrick. (2011). In vitro anti-HIV and immunomodulatory potentials of Azadirachta indica (Meliaceae) leaf extract. African Journal of Pharmacy and Pharmacology. 5. 1353- 1359. Azadirachta indica (neem) is attributed to have many ethnopharmacological properties and has been postulated to have a significant effect on CD4 counts in HIV/ AIDS subjects; however, the precise anti-retroviral mechanism is not yet known. In this study, a hydroacetone extract of A. indica leaves was investigated for its anti-retroviral and immunomodulatory potentials. The effect of the neem leaf extract on acute HIV infectivity and fusion was measured by the syncytia formation assay on HIV-1-infected C8166 CD4+ cells. The inhibitory effect of the extract on reverse transcriptase (RT) polymerase activity and HIV p24 antigen expression was evaluated in the culture supernatant. The extract was also assessed for its ability to decrease the phenotypic expression of the immune activation markers CD38 and CD69. Results from a syncytium formation assay indicated that the extract blocked HIV-1 envelope-mediated membrane fusion. The extract inhibited HIV- 1 replication in C8166 CD4+ cells in vitro by inhibiting the biochemical activity of HIV-1 reverse transcriptase, the result being a subsequent decrease in HIV p24 antigen concentration. In the effective dose range, no cytotoxicity was detected on uninfected target cells. Ex vivo, the extract exhibited a dose-dependent reduction in the levels of the immune activation marker CD38 and CD69 on phytohemagglutinin A (PHA)- stimulated human peripheral blood mononuclear cells (PBMC). The observed anti-HIV activity and immunomodulatory potentials of the extract show that neem could impart health benefits to HIV/AIDS patients, possibly by acting as fusion or reverse transcriptase inhibitors and also down-regulate hyperimmune activation.
- Chattopadhyay, Rabiranjan. (2004). Possible mechanism of hepatoprotective activity of Azadirachta indica leaf extract: Part II. Journal of Ethnopharmacology. 89. 217- 9. 10. 1016/ j. jep. 2003. 08. 006. Hepatoprotective activity of Azadirachta indica leaf extract against paracetamol-induced hepatic damage in rats has already been reported. In the present investigation, the effects of Azadirachta indica leaf extract on blood and liver glutathione, Na+ K(+) -ATPase activity, and thiobarbituric acid reactive substances against paracetamol-induced hepatic damage in rats have been studied with a view to elucidating the possible mechanism behind its hepatoprotective action. It was interesting to observe that Azadirachta indica leaf extract has reversal effects on the levels of the above-mentioned parameters in paracetamol hepatotoxicity. Possible mechanisms behind the results are discussed.
- Nagesh, Simhadri & M, Muniappan & I, Kannan & Subramanian, Viswanathan. (2018). ANTIFUNGAL ACTIVITY OF A SECONDARY METABOLITE OF AZADIRACHTA INDICA AND ITS DERIVATIVES – AN IN-SILICO STUDY. Asian Journal of Pharmaceutical and Clinical Research. 11. 175. 10. 22159/ ajpcr. 2017. v11i1. 22171. Objective: This study aimed to inhibit the 1, 3 β-glucan synthase with azadirachtin or with its derivatives by the docking method.Methods: The homology model of the protein 1, 3 β-glucan synthase was prepared with “easy modeler” using the query sequence and template, and it was validated with procheck of Ramachandran plot. The ligand was selected from the PubChem database, and the .sdf file was downloaded, which was converted to another file format with Open Babel. The files of protein and ligand were uploaded for rough docking with iGEMDOCK, and finally, the accurate docking was made with Autodock Vina. The docked poses were visualized with PYMOL and then saved. The derivatives of the ligand were generated with SWISS ADME, a free online software, and the derivative was selected for docking. Results: The results obtained from iGEMDOCK and Autodock Vina were tabulated. It was found out that the Azadirachtin and the derivatives are effective in binding 1, 3 β-glucan synthase and thereby inhibiting the formation and integrity of fungal cell wall. Conclusion: In this study, the secondary metabolite Azadirachtin and its derivatives show inhibitory action against the model protein 1 3 β-glucan synthase, and it was suggested that the external application of the ligand and its derivatives can be used because of their poor oral bioavailability.
- Maruthappan, K (2009). Hepatoprotective effect of Azadirachta indica (Neem) leaves against alcohol induced liver injury in albino rats. Journal of Pharmacy Research. Herbal drugs are traditionally used in various parts of the world to cure different diseases. The Ayurvedic and Siddha medical systems are very famous medical practices in Indian traditional medicine. The purpose of this study was to evaluate the hepatoprotective activity of A. indica using an ethyl alcohol induced liver injury in rats and probe into its mechanism of action. Liver damage was induced in Wistar rats (150- 200 g) by administering 30 % ethyl alcohol (1 ml/ 100 g b.wt.) once daily for 14 days. A. indica (1 g/ kg b. wt.) was given for 14 days. Silymarin (0.1 g/ kg b. wt.) was given as a reference drug once daily for 14 days. Levels of serum marker enzymes (AST, ALT, and ALP) were significantly (p< 0.05) increased in ethyl alcohol treated rats. Simultaneously, A. indica leaf powder and silymarin, a standard drug, significantly (p< 0.05) suppressed mainly the increase in plasma activities of AST, ALT, and ALP concentration, which are considered as markers of liver functional state. The significant (p< 0.05) decrease in the liver total protein (TP) and albumin (Alb) levels after ethyl alcohol treatment, which were reversed with A. indica. These effects were comparable to silymarin. To probe the possible mechanism by which A. indica prevents hepatic damage caused by ethyl alcohol, investigation on levels of thiobarbituric acid reactive substance (TBARS) was found to be elevated and significant (p< 0.05) decrease in glutathione reductase (GSH), superoxide dismutase (SOD) and catalase (CAT) content of liver after treatment with ethyl alcohol, which were significantly (p< 0.05) reversed by A. indica. The effects of A. indica were comparable to those of silymarin. The results of this study confirmed the hepatoprotective activity of the A. indica leaf powder.
- Baligar, Nagappa & Aladakatti, Ravindranath & Ahmed, Mukhtar & Hiremath, Murigendra. (2014). Hepatoprotective activity of the neem-based constituent azadirachtin-A in carbon tetrachloride intoxicated Wistar rats. Canadian journal of physiology and pharmacology. 92. 267- 77. 10. 1139/ cjpp- 2013- 0449. This study aimed to investigate the hepatoprotective role of azadirachtin-A in carbon tetrachloride (CCl4) induced hepatotoxicity in rats. The group allotment for the animals used in the hepatoprotective study included a vehicle treatment group, CCl4 (1 mL(kg body mass) (-1)) treatment group, silymarin (100 μg (kg body mass)(-1) day (-1)) + CCl4 treatment group, and groups treated with different doses of azadirachtin-A (100 or 200 μg (kg body mass) (-1) day (-1)) + CCl4. On the 9th day, blood was obtained for measuring the biochemical parameters, and liver tissue was obtained for pathological examination. The acute toxicity test with azadirachtin-A (500, 1000, or 2000 μg (kg body mass) (-1)) indicated no mortality after 14 days of treatment; further, there was no change in behavior, food consumption, or organ mass. However, with the higher dose, some hematological parameters showed changes. Hepatoprotective studies revealed that the CCl4 treatment group exhibited a decrease in total protein and albumin levels, whereas a significant increase in BUN, AST, ALT, and ALP levels was noticed compared with the vehicle-treated control, indicating that there was liver damage caused by CCl4. Histology and ultrastructure study confirmed that pretreatment with azadirachtin-A dose-dependently reduced hepatocellular necrosis and, therefore, protected the liver against toxicity caused by CCl4. The results from this study indicate that pretreatment with azadirachtin-A at the higher dose levels moderately restores the rat liver to normal. This study confirms that azadirachtin-A possesses greater hepatoprotective action; however, the effective concentration needs to be determined.
- Sadasivam, Poompavai & Sree, v.gowri & RamSugitha, B. (2021). Enhanced Extraction and Improved Anticancer Activity of Neem ( Azadirachta indica ) Leaves by Electroporation Technique. IETE Journal of Research. 1-11. 10. 1080/ 03772063. 2021. 1962743. Plant-based medicines have been a part of primary healthcare since time immemorial. Natural products have received increasing attention to treat several regenerative diseases due to their availability and fewer side effects than conventional drugs. Towards this, Neem, commonly known as ‘Divine Life-giving tree’, has been investigated for its efficiency against MCF7, breast cancer cell lines. Ethanolic neem extracts were analysed for qualitative phytochemical screening tests, spectral analysis, antioxidant activity, and total phenol contents. In addition, to enhance the recovery of secondary metabolites from the plant extracts, the electroporation (EP) technique is used. The effect of EP was studied by comparing with untreated extracts, which exhibit antioxidant activity (∼96% increase) and total phenol contents (∼12.51 % increase) than untreated extracts. This indicates that electroporated extract (EE) exhibited higher antioxidant and phenolic activity than other extracts. Furthermore, different concentrations of untreated and electroporated neem extracts were used to study the anti-cancer activity. To enhance the uptake of extracts against cell membranes, electrical pulses of EP1 = 1200 V/cm, 100 s, 8 pulses and EP2 = 500 V/ cm, 20 ms, 8 pulses were used. The results indicate cell viabilities of 35 % with untreated extract only, 5.6 % with EE, 3.17 %, and 2.49 % with EP1 + EE extract and EP2 + EE extract, respectively, indicating the potential of the synergy of electrical pulses + EE. The viability was lowered by 5– 6 times after 72 h. This treatment is more appropriate to achieve maximum cell death, thereby reducing the side effects of conventional drugs in treating breast cancer.
- Nahak, Dr. Gayatri & Sahu, Rajani. (2010). Antioxidant activity in bark and roots of Neem (Azadirachta indica) and Mahaneem (Melia azedarach). Continental J. Pharmaceutical Sciences. 4. 28- 34. This study aimed to investigate the antioxidant activity of the multi-solvent extracts (aqueous, methanolic and ethanolic) of Root and Bark of two Medicinal plant i.e. Azadirachta indica A. Juss and Melia azedarach of Meliaceae family using 2, 2- diphenyl- 1- picryl- hydrazyl (DPPH) – scavenging assay. The dry powder of the Root and Bark of the two-neem tree was extracted using Soxhlet extraction followed by vacuum rotary evaporator methods. The extracts were tested for antioxidant activity using- DPPH-scavenging assay. Total phenol contents of extracts were also determined by the Folin-Ciocalteu reagent method. Experimental results revealed the highest fraction of crude extract, phenol content, as well as antioxidant activity in Barks and Roots of Mahaneem (Melia azedarach) in comparison to Neem (Azadirachta indica). The total phenolic concentration of the Bark and root of Melia showed a positive correlation with antioxidant capacity. Similarly, IC50 values in Bark and Root of Mahaneem were as low as those of Ascorbic acid. The plant Mahaneem and its plant parts may be exploited for clinical medicine as a potent factor because of their high antioxidant activity.
- Bharat, Pokhrel & Sagar, Rijal & Sulav, Raut & Pandeya, Ankit & eya. (2015). Investigations of antioxidant and antibacterial activity of leaf extracts of Azadirachta indica. African Journal of Biotechnology. 14. 3159- 3163. 10. 5897/ AJB2015. 14811. Active ingredients of medicinal plants have been used to cure several human diseases. Azadirachta indica is one of the most versatile medicinal plants, having a wide spectrum of biological activity due to the presence of a large number of bioactive compounds. The present study was conducted to evaluate antimicrobial and antioxidant efficiency and phytochemical screening of A. indica leaf extract using methanol as a solvent. A qualitative phytochemical screening was performed for the detection of various phytochemicals. Then, the quantitative determination of total phenols, flavonoids, and proanthocyanidins was done and expressed in terms of gallic acid and rutin equivalent. Total phenolic, flavonoid, and proanthocyanidin content were found to be 85.9± 4.0, 104.9± 5.5, and 65.4± 13.9 mg/g of plant extract, respectively. Also, the antibacterial activity was performed using six different bacterial strains: Escherichia coli (ATCC 25922), Staphylococcus aureus (ATCC 25923), Salmonella typhi (ATCC 14028), Klebsiella pneumoniae (ATCC 700603), Pseudomonas aeruginosa (ATCC 27853), and Proteus vulgaris (ATCC 35659). It was found that the maximum zone of inhibition of 22±3 mm was shown against S. aureus using 700 μg of plant extract. Similarly, the antioxidant activity of the methanolic extract of the plant was also determined, and it was found that the maximum inhibition obtained was 71.23 % when 500 μg of the plant extract was used.
- Thakurta, Prarthana & DeBhowmik, Poulami & Mukherjee, Souryadeep & Hajra, Tapas & Patra, Amarendra & Bag, Prasanta K. (2007). Antibacterial, antisecretory, and antihemorrhagic activity of Azadirachta indica is used to treat cholera and diarrhea in India. Journal of Ethnopharmacology. 111. 607- 12. 10. 1016/ j. jep. 2007. 01. 022. Indigenous uses of Azadirachta indica A. juss (Maliaceae) (locally known as neem) leaves in different parts of India for curing gastrointestinal disorders such as diarrhea and cholera are widespread. The objective of the present study was to evaluate the antibacterial and antisecretory activity of neem extract against Vibrio cholerae, a causative agent of watery diarrhea, such as cholera. The methanol extract of neem leaf was tested for its antibacterial, antisecretory, and antihemorrhagic activity against Vibrio cholerae. Azadirachta indica extract had significant antibacterial activity against the multi-drug-resistant Vibrio cholerae of serotypes O1, O139, and non-O1, non-O139. The minimum inhibitory concentration reached by 50 % (MIC 50) and 90 % (MIC 90), and the minimum bactericidal concentration for the extract were 2.5, > 5, and 10 mg/ml, respectively. Neem extract showed antisecretory activity on Vibrio cholerae induced fluid secretion in the mouse intestine with inhibition values of 27.7 %, 41.1 %, 43.3 %, 57.0 %, and 77.9 % at doses of 100, 200, 300, 450, and 1800 mg/kg, respectively. Oral administration of the extract inhibited hemorrhage induced by Vibrio cholerae in the mouse intestine at a dose > of = 300 mg/ kg or greater. The results obtained in this study give some scientific support to the use of neem employed by the indigenous people in India for the treatment of diarrhea and the dreadful disease cholera.
- Pedroza, David & Benjamín, Serrano-Gallardo & Edith, Escobar-Ávila & Delia, Alma & Nava-Hernández, & Patricia, Martha & María, Vega-Menchaca & Carmen, Del. (2017). HIV-1 infection inhibition by neem (Azadirachta indica A. Juss.) leaf extracts and Azadirachtin. Indian journal of traditional knowledge. 16. 437- 441. Mexico is a country with a strong attachment to the use of traditional medicine, which is the heritage of pre-Hispanic ethnic groups of Mexican territory that are still present all across the country. The Mexican markets, dedicated exclusively to trade medicinal plants, have facilitated the use, getting, and importation of plants from other regions of the world, such as neem, which has been used for many health conditions, both non-communicable and infectious diseases, such as cancer, diabetes, bacterial, parasitic, and viral infections, even the infection with human immunodeficiency virus. , The objective of this study was to evaluate HIV-1 infection inhibition by neem leaf extracts and neem compounds. Cytotoxicity of aqueous and ethanolic neem leaf extracts and Azadirachtin and Limonene compounds was evaluated in CEM T-cells at concentrations of 1 ppm, 10 ppm (extracts); 1 µM, 10 µM (compounds). Only the aqueous extract concentration of 1 ppm and Azadirachtin at 1 µM and 10 µM concentrations allowed a cell viability of 100 % compared with controls, p > 0.05. Based on the results of cytotoxicity, we proceeded to evaluate the HIV infection inhibition with the aqueous extract at a concentration of 1 ppm and Azadirachtin at both concentrations. Inhibition percentages greater than 50 % were obtained and showed to be significant compared to controls p < 0.001 This work evidenced the HIV infection inhibition by aqueous neem leaf extracts and Azadirachtin; even though the antiretroviral mechanism is not completely understood. Furthermore, more studies need to be conducted in order to identify the active compound responsible for the anti- HIV activity described in the aqueous extract.
Recent Research on Akasha Nimba (Millingtonia hortensis)
- Chaiyasit, Sittiwet. (2009). Antimicrobial Activities of Millingtonia hortensis Linn. Flowers Essential Oil. Journal of Pharmacology and Toxicology. 4. 41- 44. 10. 3923/ jpt. 2009. 41. 44. Millingtonia hortensis Linn. flowers have been extracted for essential oil using vapor distillation, with 0.5- 2 % yield. The essential oil of M. hortensis Linn. was tested against various species of bacteria. The agar diffusion susceptibility test showed an inhibitory effect on 6 out of 10 tested strains. The growth of 4 gram-positive bacteria (S. aureus ATCC 25923, S. epidermidis ATCC 12228, B. subtilis ATCC 6633, and L. plantarum ATCC 14917) and 2 gram-negative bacteria (E. coli ATCC 25922 and P. vulgaris ATCC 13315) was inhibited by M. hortensis Linn. flower essential oil. The MICs (minimal inhibitory concentration) of M. hortensis Linn. flower essential oil are 0.5- 2 and 1- 4 ml L- 1, respectively. In this study, M. hortensis Linn. flower essential oil showed broad-spectrum antimicrobial activity at low concentration.
- Jetty, A. & Iyengar, D. S. (2000). Antimicrobial Activity of Millingtonia Hortensis Leaf Extract. Pharmaceutical Biology. 38. 157- 160. 10. 1076/ 1388-0209- 28200004- 293821- 1FT157. Polar extracts of the leaves of Millingtonia hortensis showed good antimicrobial activity. Twenty different bacterial strains and two yeast cultures were used. The aqueous alcohol extract showed good activity against all microbes tested, particularly Escherichia coli and Salmonella typhimurium, both Gram-negative bacteria, with MIC values of 6.25 µg/ml. The activity is compared with known antibiotics such as gentamycin and nystatin.
- Arumugam, Janaki & Muthu, Babu. (2017). Phytochemical screening of antioxidant and antibacterial activities of Millingtonia hortensis (L). International Journal of Current Pharmaceutical Review and Research. Herbal medicines are in great demand in both developed and developing countries because of their enhanced bio-efficacy and minimal side effects. In the present investigation, the leaf extracts of the plant Bauhinia tomentosa were evaluated for their cytotoxicity and antioxidant properties. The phytocompounds responsible for the bioactivity were analysed qualitatively and quantitatively. Phytochemical screening of the leaf extracts showed the presence of steroids, alkaloids, saponins, coumarins, flavonoids, phenols, and amino acids. GC-MS analysis revealed the presence of nine major phytocompounds in the methanol leaf extract. Antioxidant efficacy of the leaf extracts was analysed in vitro by DPPH and superoxide radical assays, and their cytotoxicity was evaluated on the MCF-7 cell lines. The leaf extracts were non-toxic, and their potent antioxidant activity and anticancer activity may be due to the presence of phytocompounds such as flavonoids and phenols.
- Puri, S, & Sharma, P.D. (2007). Antifungal activity of Millingtonia hortensis. Indian Journal of Pharmaceutical Sciences. 69. 10.4103/0250-474X.36959. Antifungal activities of different extracts of Millingtonia hortensis were investigated against various fungal pathogens. Methanol extract was found to have stronger activity than fluconazole against yeast-like fungi: 4-fold against Candida krusei with a 4 µg/ml minimal inhibitory concentration and 2-fold (MIC- 2 µg/ml) against Sacharomyces cerevisiae, though it showed the same activity as fluconazole against Candida glabrata. Aqueous extract also exhibited 4- fold stronger activity against Candida krusei (MIC- 4 µg/ ml) and 4- fold (MIC: 2 µg/ ml) against Sacharomyces cerevisiae. Chloroform and ethyl acetate extracts showed lower activities against all fungal pathogens except for Candida krusei, compared with the standard. Against the filamentous fungus, Trichosporon cutaneum, all extracts showed less activity than the standard.
- Babitha, S & Banji, David, & Banji, Otilia. (2012). Antioxidant and hepatoprotective effects of flower extract of Millingtonia hortensis Linn. on carbon tetrachloride-induced hepatotoxicity. Journal of pharmacy & bioallied sciences. 4. 307- 12. 10. 4103/ 0975- 7406. 103258. Millingtonia hortensis Linn is an abundant source of flavonoids, which might be beneficial in protecting liver tissue from injury. The hepatoprotective and antioxidant potential of ethanolic extract of M. hortensis on carbon tetrachloride (CCl (4)) induced hepatotoxicity, and the possible mechanism involved therein was investigated in rats.
- Preliminary phytochemical studies were carried out to determine the total phenol and flavonoid contents. 30 adult Wistar rats were allocated into 5 groups. Control group received vehicle, group-2 received CCl (4) alone (1 ml/ kg body weight, intraperitonially), groups 3 – 5 received the ethanolic flower extract in 2 dose levels (200 and 400 mg/ kg) and Curcumin (100 mg/kg) as a standard for 8 days orally, followed by CCl (4) as a single dose on the 8 (th) day. 48 hours later, blood was withdrawn, serum was subjected to biochemical assessments, and liver homogenate was examined for lipid peroxides, glutathione, superoxide dismutase, catalase, and total protein levels. Furthermore, hepatic tissues were subjected to histopathological studies. CCl (4) treatment produced a profound increase in the levels of malondialdehyde, hepatic marker enzymes, and bilirubin content compared with the control (P < 0.05). Pre-treatment with the flower extract of M. hortensis significantly enhanced the levels of endogenous antioxidants and reduced the levels of hepatic marker enzymes in relation to the CCl (4) treated group (P < 0.05). Balloning degeneration and fatty changes in hepatocytes were prevented by pre-treatment with the flower extract. The antioxidant nature of the flower extract of M. hortensis could be responsible for averting damage to the liver.
- Kumar, M. & Ravichandran, N. (2011). Cytotoxicity and antimicrobial studies of the stem bark of Millingtonia hortensis Linn. International Journal of Pharmacy and Pharmaceutical Sciences. 3. 247- 249. The present study aims to explore the cytotoxic potential and antimicrobial capacity of the aqueous extract of the stem bark of Millingtonia hortensis Linn. The aqueous extract of the stem bark of Millingtonia hortensis Linn is tested against the Human cervical cancer cell line by MTT Assay. The antimicrobial capacity of the extract is evaluated by means of the agar diffusion method using 12 strains of microbes. The extract is found to be a poor cytotoxic and antibacterial agent; however, it is found to be an effective antifungal agent. The isolation of phytoconstituent from the stem bark of Millingtonia hortensis Linn may lead to a novel antifungal agent rather than an antibacterial or cytotoxic agent.
- Tansuwanwong, Siwapong & Yamamoto, Hiroyuki & Imai, Kohzoh & Vinitketkumnuen, Usanee. (2007). ANTIPROLIFERATIVE EFFECT ON COLON CANCER CELL LINES BY AQUEOUS EXTRACT FROM THE BARK OF MILLINGTONIA HORTENSIS. 46. Millingtonia hortensis is a traditional medicinal plant widely used in Southeast Asia. This study focused on the antiproliferative effect when comparing aqueous extract and ethanol extract from the bark of M. hortensis using human colon cancer cell lines, DLD-1, HCT 15, SW48, and SW480. In in vitro experiments, the MTT method was used to determine the antiproliferative effect of M. hortensis extract on colon cancer cells. An aqueous extract of M. hortensis significantly reduced the proliferation rate of colon cancer cell lines in a dose-dependent manner. However, no antiproliferative effect was observed by the ethanol extract of M. hortensis. This finding indicated that only aqueous extract from the bark of M. hortensis can inhibit colon cancer cell proliferation, and its mechanism is now under investigation. Chiang Mai Medical Journal 2007; 46 (2): 61- 66.
- Jumnongprakhon, Pichaya & Pinkaew, Decha & Phuneerub, Pravaree. (2021). The antiaging property of the aqueous extract of Millingtonia hortensis flowers in aging neurons. Journal of Advanced Pharmaceutical Technology & Research. 12. 14. 10. 4103/ japtr. JAPTR_ 187_ 20. Cellular senescence is the key mediator of cellular dysfunction before undergoing degenerative disease, such as Alzheimer’s disease. The aging process was mainly mediated by the overactivation of senescence-associated β-galactosidase (SA-β-gal) enzyme, which led to several negative responses, including intracellular reactive oxygen species (ROS) production, cellular senescence regulation, and death, which contributed to encouraging synaptic loss. Thus, in the recent work, we evaluated the in vitro effects of aqueous extract of Millingtonia hortensis L. (MH) from the flowers in hydrogen peroxide (H2O2)- induced senescence in SK-N-SH cells. Herein, we demonstrated that MH significantly increased cell viability and decreased both of apoptotic cells and ROS production in a dose-dependent manner comparing to aging group (P < 0.01) using 3- (4, 5- dimethylthiazol- 2- yl)- 2, 5-diphenyltetrazolium bromide, flow cytometry, and ROS assay. Furthermore, the number of SA-β-gal-positive cells was also reduced in MH treatment (P < 0.01), together with the promotion of Sirt-1 protein. Importantly, MH also promoted synaptic plasticity by decreasing acetylcholinesterase activity and increasing synaptophysin expression in aging neurons compared to the aging group (P < 0.01). Hispidulin (the active ingredient in MH) was also revealed to have similar effects to MH. Therefore, we suggested that MH might be beneficial for neurodegenerative diseases caused by aging.
- Kumar, M. & Kavimani, S. (2014). Anthelmintic activity of Millingtonia hortensis Linn. F. stem bark on Indian adult earthworm. Der Pharmacia Lettre. 6. 89- 91. Millingtonia hortensis Linn. F (Bigoniaceae) is a traditional medicinal plant widely used in Southeast Asia for its fragrant flowers. It is commonly known as the Cork tree, Akash neem, and Neem chameli. The present study aims at exploring the anthelmintic potential of aqueous extract of the stem bark of Millingtonia hortensis Linn. F. An Anthelmintic study was carried out using the Indian earthworm, Pheretima posthuma. Anti-helmintic activity of Millingtonia hortensis aqueous extract was evaluated at 10 mg/ ml, 20 mg/ ml, 30 mg/ ml, 40 mg/ ml, and 50 mg/ ml, using piperazine citrate and piperazine hexahydrate as standards. The time taken for paralysis and death was calculated for all the groups. Millingtonia hortensis aqueous extract exhibited less anthelmintic activity as compared to the standard drugs. The study concludes that Millingtonia hortensis aqueous extract is not a suitable drug of choice for anthelmintic properties.
- Tansuwanwong, Siwapong & Hiroyuki, Yamamoto & Imai, Kohzoh & Vinitketkumnuen, Usanee. (2006). Induction of apoptosis in RKO colon cancer cell line by an aqueous extract of Millingtonia hortensis. Asian Pacific journal of cancer prevention: APJCP. 7. 641- 4. Millingtonia hortensis is an important medicinal plant in Southeast Asia, used for the treatment of asthma, sinusitis, and as a cholagogue and tonic. This study aimed to compare the effects of aqueous and ethanol extracts of Millingtonia hortensis on the induction of apoptosis in an RKO human colon cancer cell line. The viability of RKO cells was assessed by MTT reduction assay. The aqueous extract, but not the ethanol extract of M. hortensis, inhibited cell growth and proliferation in a dose- and time-dependent manner. Apoptotic cells were determined by flow cytometry and DNA fragmentation assay. Apoptotic cell numbers increased in a dose-dependent manner after treatment with aqueous extract. DNA ladders were clearly observed in RKO cells treated with 200, 300, and 400 g/ ml of the aqueous extract of M. hortensis for 48 h. These results indicate that the aqueous extract of M. hortensis inhibited cell proliferation in an RKO colon cancer cell line via the apoptosis pathway.
Rasa Panchaka of Nimba
| Rasa (Taste) | Tikta (Bitter), Kashaya (Astringent) |
| Guna (Virtue) | Ruksha (Dry), Laghu (Light) |
| Virya (Potency) | Sheeta (Cold Potency) |
| Vipaka (Post-Digestion) | Katu (Pungent) |
Dosha Karma of Nimba
Kapha Pitta Shamaka
Kapha Shamaka because of its Katu Vipaka and Kashaya, Tikta Rasa.
Pitta Shamaka due to Sheeta Virya, Kashaya, and Tikta Rasa.
Karma (Actions) of Nimba
Kandu Ghana, Kustha Ghana, Jantu Ghana, Vrana Ropana, Vedna Sthapana, Yakrit Uttejaka, Rochana, Grahi, Krimi Ghana, Rakta Shodhaka, Sotha, Garbhashya Uttejaka, Ama Pachana, Jwara Ghana, Vishma Jwara Ghana, Nalya, Chakshushya, Shrmahara, Visha Ghna, Pitta Shamaka, Keshya, Rasayana, Balya.
Patra (Leaf): Krimighna, Netrya, Visaghna, Kusthagna, Rucikara, Vranaghna, Kasahara, and Swasahara.
Twak (Bark): Kusthaghna, Krimighna, Sramahara, Trisnahara, Jwaraghna, Chardighna, Kandughna, Pramehahara, Rucikara, Sothahara, and Rakta Sodhaka.
Phala (Fruit): Kusthaghna, Arsoghna, Krimighna, Bhedana, Mehahara, and Gulmanasaka.
Puspa (Flower): Krimighna, Visaghna.
Bija (Seed): Krimighna and Kusthaghna.
Prayogarha Vyadhi (Therapeutic Indications) of Nimba
Kandu, Kustha, Tvak Vikara, Kshudra Roga, Vrana, Granthi, Vidridhi, Apachi, Nadi Vrana, Ganda Mala, Vishphota, Sheta Pitta, Udarda, Kesha Vikara, Khalitya, palitya, Yakrit Vikara, Krimi Roga, Grehani, Vivandha, Arsha, rakta Arsha, Rakta Vikara, Upadansha, Phiranga Roga, Prameha, Madhu Meha, Sura Meha, Balya, Netra Roga, Netra Abhushyanda, Kasht Artava, Kasa, Swasa, Danta Roga, Yoni Roga.
- Puspa (Flower) – Krimi and Visa Roga.
- Patra – Kustha, Krimi, Netra roga, Aruci, Kasa.
- Leaf – Swasa, Visaroga, and Vrana
- Twak (Bark) – Kustha, Krimi, Kandu, Prameha, Aruci, Raktadusti, Irisna, Srama, Chardi, and Sotha.
- Phala (Fruit) – Kustha, Arsas, Krimi, Prameha, and Gulma.
- Bija (Seed) – Krimi and Kustha.
Aamyik Paryog (Therapeutic uses) of Nimba
Jwara (Fever):
- Vomiting should be induced in patients having a burning sensation and fever with the leaf juice of nimba mixed with honey and liquid jaggery. (Sushruta Samhita Uttara Tantra. 39/ 282)
- Fumigation with leaf, root, flower, fruit, and bark mixed with ghee is also useful. (Kashyapa Samhita. Page. 171)
Rakta Pitta (Intrinsic haemorrhage): Patola, nimba, tender leaves of vata, plaksa, and vetasa are useful as vegetables. (Bhava Parkasha Chikitsa. 9. 18)
Rakta Arsha (Bleeding piles): The seed kernel is put within a bifurcated big radish and cooked by closed heating. Then it is pounded and made into pills. It destroys piles. (Siddha Bhaishjya Mannimala. 4/ 238)
Vrana (Wound): One should take juice of the leaves of dhattüra or nimba mixed with honey. It is an excellent anthelmintic. (Bhava Parkasha Chikitsa. 7/ 24)
Shotha (Oedema): Tub-bath should be taken with the decoction of nimba, ankotha, eranda, tarkari, kutaja, karanja, and banana (all leaves). (Kashyapa Samhita Page. 344)
Udarad (Urticaria): By the regular use of the leaves of nimba and amalaki (fruit) mixed with ghee, urticaria and skin diseases are alleviated. (Vrinda Madhava. 52/ 8, Chakra Dutta. 51/ 9
Vatarakta (Gout):
- One who swallows the paste of nimba 80 gm in the morning, keeping on a diet of wholesome items and ghee, becomes free from severe vatarakta. (Siddha Bhaishjya Mannimala. 4/ 837)
- Decoction of patola and nimba leaves mixed with honey pacifies vätarakta. Nimba leaves pounded with sour gruel should be applied externally. (Harita Samhita. 3. 23. 7- 8)
Kustha (Skin disorder)
- The combination of nimba and patola is efficacious in kustha in various forms. (Charaka Samhita Chikitsa Sthana. 7/ 97- 99)
- In kustha, if the part is wounded and eaten by maggots, nimba and vidanga with cow’s urine should be used as bath, intake, and anointment. (Charaka Samhita Chikitsa Sthana. 7/ 157)
- In case of the emergence of maggots, one should take the decoction of nimba or arka, alarka, and saptaparna. In parts eaten by maggots, paste of karavira root and vidanga with cow’s urine is useful. (Sushruta Samhita Chikitsa Sthana. 9. 51- 52)
- Pancha Nimba Churna. (Vrinda Madhava. 51/ 60- 68)
- One who uses one hundred nimba leaves pounded with water for a year, keeping on a diet of flour, becomes free from severe types of kustha. (Gada Nigreha. 2/ 36/ 99)
- One who takes haritaki and nimba or nimba and amalaka for a month overcomes all types of kustha. (Gada Nigreha. 2/ 36/ 87)
- Nimba juice should be used according to your strength, taking into account your diet. On its digestion, of ghee and cereals with little soup. By this, the person attains a handsome body. (Vanga Sena kustha. 103)
- Fresh nimba leaves should be swallowed with cold water in the morning for a month, abstaining from an unwholesome diet. Thus, kustha is destroyed. (Siddha Bhaishjya Mannimala. 4/ 836)
Prameha (Diabetes):
- Decoction of nimba is the specific remedy for surameha. (Sushruta Samhita Chikitsa Sthana. 11/ 9)
- Decoction of bark, leaves, root, fruit, and flowers of nimba, aragvadha, saptaparna, murva, kutaja, katphala, and palasa destroys all types of prameha. (Sushruta Samhita Chikitsa Sthana. 11/ 8)
Amla Pitta (Acid gastritis)
- Panchanimba one part, Vriddhadaruka two parts, and parched grain flour ten parts mixed with sugar should be taken with cold water. It alleviates colic caused by pitta and kapha. Its powder taken with honey alleviates severe amlapitta. (Vrinda Madhava. 53. 18- 19)
- Trishna (Excessive thirst): The patient should vomit with a hot decoction of nimba leaves. (Sushruta Samhita Uttara Tantra. 48. 21, Vrinda Madhava 16/ 5)
Daha (Burning sensation)
- Froth coming out of the leaves of badari, nimba, or upodikā should be applied externally on the affected part. (Charaka Samhita Chikitsa Sthana. 24/ 160)
- By external application of the froth of nimba, thirst, burning sensation, and mental confusion are pacified. (Vaidyak Jeevan. 1/ 28)
- Shiro Pidika (Head-boils): After blood-letting, boils should be sprinkled with nimba decoction. (Sushruta Samhita Chikitsa Sthana. 20/ 27)
Kustha (Skin diseases):
- Local application of the juice of dhattura, nimba, and betel leaves separately destroys skin diseases such as eczema, ringworm, etc. (Sharangdhara Samhita, 3. 11. 52- 53)
- Padminikantaka: Anointment of the paste of nimba and aragvadha is useful. (Sushruta Samhita Chikitsa Sthana. 20/ 39, Ashtanaga Sangraha Uttara Tanttra. 37/ 6, Vrinda Madhava. 57/ 20)
- Intake of ghee cooked with nimba decoction and mixed with lime is efficacious. (Ashtanga Hridya Uttara Tantra. 24/ 34)
Paalitya (Greying of hair):
- Nimba oil should be taken as snuff for a month, while on a milk diet. (Ashtanaga Hridya Uttara Tantra. 24/ 34, Vrinda Madhava. 57/ 93, Sharangdhara Samhita. 2. 9. 152)
- Seeds of nimba are impregnated with the juice of bhrigaraja and the decoction of bijaka, and oil is extracted. It is taken as snuff, along with the diet of milk and cereals. It eradicates the disease. (Vrinda Madhava. 57/ 92)
Mutra Kriccha (Dysuria): Rachis of nimba leaves is pounded and put in water in an earthen vessel in the evening. This cold infusion is taken in the morning. It relieves dysuria. (Siddha Bhaishjya Mannimala. 4/ 538)
Vrana (Wounds)
- Decoction of nimba leaves cleans the wound. (Charaka Samhita Chikitsa Sthana. 25/ 84)
- Nimba leaf mixed with honey acts as a cleansing agent. Both of them, added with ghee, promote healing. (Sushruta Samhita Chikitsa Sthana. 1/ 68)
- Paste of nimba leaves and sesamum mixed with honey cleanses wounds, while mixed with ghee, it acts as a healing agent. The same is in respect to barley paste. (Vrinda Madhava. 44/ 28)
- The paste of nimba leaves, by external application, cleanses and heals wounds, while by intake it alleviates vomiting, kustha, disorders of pitta and kapha, and worms. (Sharangdhara Samhita. 2. 5. 5)
- Nimba mixed with hingu should be applied. (Bhava Parkasha Chikitsa. 47/ 69)
Netra Vikaar (Eye diseases):
- Juice of the nimba fruit is rubbed in an iron pan, and when slightly solidified, it is applied to the lids. It removes discharge from the eyes. (Sharangdhara Samhita. 3/ 13/ 35)
- Warm paste of sunthi and nimba leaves, added with a little rock salt, should be applied to the eyes. It removes inflammation, itching, and pain. (Sharangdhara Samhita. 3. 13. 29)
- Powder of nimba leaves mixed with lodhra powder is kept in a cotton pouch and dipped in water. The extract so obtained is dropped in the eyes. It alleviates diseases of the eye. (Banga Sena netra. 117)
Pradara (Leucorrhea): In pradara caused by kapha, one should take nimba and guduci with wine. (Charaka Samhita Chikitsa Sthana. 30/ 99)
Stanya Shodhana (As galacto-depurant): Soups prepared of nimba, tips of vetra, patola, vartaka, and amalaka added with trikatu and rocksalt should be given to purify breast milk. (Charaka Samhita Chikitsa Sthana. 30/ 259)
Vishakta (Poisons):
- Nimba seeds taken with hot water neutralise the poison immediately. (Harita Samhita. 3. 56. 11)
- One piece of peacock’s flesh mixed with two leaves of nimba should be taken when the sun comes in the Mesa constellation (month of Vaisakha). By this, the person is protected from poison for a year. (Vrinda Madhava. 68/ 2)
- Kamala (Jaundice): One suffering from jaundice should take a cooled decoction of triphala or gudüci or darvi, or nimba mixed with honey in the morning. (Charaka Samhita Chikitsa Sthana. 16/ 63)
Dhupana Dravya (For fumigation):
Five parts (leaf, root, flowers, fruits, and bark) of nimba mixed with ghee are used for fumigation. It wards off diseases. (Kashyapa Samhita Dhupakalpa)
Fumigation with guggulu, vaca, kustha, hide of elephant and sheep, and nimba leaves mixed with honey and ghee alleviates fever, particularly in children. (Vanga Sena Balaroga. 27)
Dant Gat Roga (Diseases of teeth):
- Decoction of the root bark of nimba alleviates diseases of the teeth. (Harita Samhita. 3/ 46/ 14)
- It is also prescribed as a brush. (Sushruta Samhita Chikitsa Sthana. 24/ 6)
Hridya Roga (heart disease): In heart disease caused by kapha, the patient should vomit with the decoction of nimba and vacha. (Vanga Sena Hridayaroga. 26)
Paachak Drvya (As specific digestive): In case of indigestion caused by (over-eating) madhuka, bilva, rajadana, parusaka, kharjura, and kapittha, and also ghee and buttermilk, nimba seed should be taken. (Bhava Parkasha Chikitsa. 6/ 131)
Yoni Roga (Disorders of the vagina): By washing frequently with the decoction of nimba and fumigating with nimba bark, the vagina becomes free from foul smell and sliminess and gets contracted. (Gada Nigeha. 6. 9. 14)elieved by putting the juice of punarnava into the vagina. (Gada Nigreha. 6. 6. 15)
Benefits of Nimba
- The drug Nimba (Azadirachta indica A. Juss.) is anthelmintic, antiseptic, bitter, deodorant, diuretic, emmenagogue, and febrifuge. It is used in blood disorders (impurities), consumption, and eye diseases.
- Neem is useful in intermittent fevers as well as persistent low fever, leprosy, scrofula, skin diseases, ulcers, and wounds.
- The active principle Nibmidin from the bark and the oil of Neem was found useful in tropical eosinophilia.
- Nimba is chiefly used in several skin affections (tavgdosa and kudra roga).
- The bath with water boiled with leaves (nimba patra snana) is the most common and effective measure for treating skin diseases.
- Leaves paste is applied to boils, ulcers, abscesses, glandular inflammation, and other similar ailing conditions.
- In sinus (nadivrana) and scrofula (apaci), the Nimba varti is applied, made with oil of Nimba.
- Oil is applied to rheumatic joint swelling and other diseases.
- Seeds are ground and applied to hair for destroying sira krmi (yuka- liksa, etc.).
- In the greying of hair (palitya) and khälitya, a snuff of seed oil is recommended.
- Leave juice or its foam is suggested to be applied over the affected body part.
- The seed oil (nimba taila) is used in diabetes (madhu-meha).
- Nimba taila picu is suggested to be kept into vagina during coitus (sambhoga-maithuna) for avoiding conception which is a local contraceptive with promising results and effective administration carrying base of classical texts as well as pharmacological and biological, and experimented support with the trials on couple subjects, adopting contraceptive measure of Nimba tail application and showing encouraging reports of action as an anti- fertility drug.
- The seed powder is given in gynaecological diseases (stri roga) and also in painful or difficult delivery (kastaprasava).
- The bark juice or decoction is given for cough (kasa). Bark is given in fevers, especially malarial and periodic fevers.
- The diseases caused by blood impurity, syphilis, and gonorrhoea are treated with Nimba.
- Bark juice mixed with honey is given for vomiting, aruchi, grahani, worms, and liver disorders.
- Nimba is recommended in amlapitta (hyper acidity and peptic ulcer) and kaphapittaja chardi. Seeds are given for eradicating piles or haemorrhoids (as arsoghna drug) as an effective remedy.
- Seeds are also given for constipation.
- Almost all the parts of Nimba (tree) are medicinal and used as preventive as well as curative remedies for a large number of diseases through a wide range of recipes and formulations prepared and administered externally and internally with suitability and clinical requirement out of rich therapeutics employing Nimba in medical systems and traditions, including tribal herbal practices. Nimba is a common, dependable, and convenient household medicine, health protector, and useful plant remedy among folks and also urban people. The wide-ranging, multifarious, and poly-utility of Nimba makes it the most popular and credible plant source in environment, pollution, drugs, health care, cosmetics, insecticides, industry, pesticides, manures, plantation, and various fields, which practically support Nimba occupying a leading place and separate identity nowadays.
Benefits of Nimba on Different Systems of Bodies
External Uses:
- Leaves and bark are antimicrobial, vrana pachan, vrana shodhan, remove foul smell, reduce burning sensation, and itching.
- Seed oil – wound healing, antileprotic, analgesic, therefore it is used in abscess, lymphadenitis, ulcer (lepa with crushed leaves is applied.).
- In pruritus, a hot water bath with decoction of neem leaves is given; neem oil is also applied as a massage.
- Chronic T.B. lymphadenitis and fistulae are treated by wicks dipped in neem oil.
- In joint swelling and inflammatory arthritis, massage is useful. Application of ground seed is done to control lice or other microbes on the scalp. Nimba tail nasya is used in psoriasis and baldness.
- Neem leaves are rubbed all over to reduce burning. A poultice of leaves is tied over the abscess.
Digestive System:
- By its astringent and bitter properties, it improves taste and is constipative.
- Fruit is purgative.
- Leaves are anthelmintic and stimulate liver functions.
- Its bark decoction with honey is useful in jaundice, anorexia, vomiting, dysentery, intestinal worms, and liver diseases.
- Ointment prepared from seeds is applied in piles. Fruits are useful for constipation.
Respiratory System:
- Its property of tikta reduces the kapha from the respiratory passage.
- Leaves are more useful in excessive mucous secretion.
- Bark decoction is used for chronic cough. 30-60 cc of liquid collected from the trunk is given in TB and leprosy.
Urinary System: It is effective in kaphapittaj prameha (diabetes).
Reproductive System:
- Nimba seed is a uterine stimulant.
- Seed powder is used in dysmenorrhoea and puerperium.
- Continuous use of leaves leads to a decrease in the dhatus of the body, especially shukra.
- The juice of the leaves should be given immediately after delivery to postpartum women as it is a uterine tonic.
- Since it is excreted in human milk, it is useful in preventing cough and skin diseases in infants (so it is called balant nimba).
Skin: It is useful in all skin conditions, especially in burning sensations.
Satmikaran:
- In general debility, young leaves and gum are useful.
- The concept behind chewing nimba leaves on the Marathi New Year is to prevent kapha diseases.
- Nimba Madya (waters discharged from nimba) is useful in emaciation and TB. Nimba is the best rasayana in Medo Roga (Fat disorders). The juice of the leaves is very useful in syphilis.
Temperature: Antipyretic, Amapachak and prevent intermittent heat. Also useful in kaphaj jwar and malarial fever.
Eyes: Tender leaves and flowers are useful in many skin disorders.phtheria, etc.
Matra (Therapeutic Administration and Dosage) of Nimba
Swarasa (Juice): 10-20 ml
Kalka (Paste): 10-20 grams
Kashaya (Decoction): 50-100 ml
Churna (Powder): 2-4 grams
Taila (Oil): 5-10 drops

Have A Health Issue?
Consult Online
- Dr. Sahil Gupta (B.A.M.S., M.H.A.)
Ayurvedic Allergy Specialist
CEO & Founder of IAFA®
Classical Reference of Nimba
Bhava Prakasha Nighantu Karpuradi Varga- 93
Synonyms
निम्बः स्यात्पिचुमर्दश्च पिचुमन्दश्च तिक्तकः |
अरिष्टः पारिभद्रश्च हिङ्गुनिर्यास इत्यपि ||
Bhava Prakasha Nighantu Karpuradi Varga- 94
Properties and actions
निम्बः शीतो लघुर्ग्राही कटुपाकोऽग्निवातनुत् |
अहृद्यः श्रमतड्कासज्वरारुचिकृमिप्रणुत् ||
व्रणपित्तकफच्छर्दिकुष्ठहृल्लासमेहनुत् |
Bhava Prakasha Nighantu Karpuradi Varga- 95
Nimba Patra
निम्बपत्रं स्मृतं नेत्र्यं कृमिपित्तविषप्रणुत् ||
वातलं कटुपाकञ्च सर्वारोचककुष्ठनुत् |
Bhava Prakasha Nighantu Karpuradi Varga- 96
Nimba Phala
निम्बफलं रसे तिक्तं पाके तु कटुभेदनम् |
स्निग्धं लघूष्णं कुष्ठघ्नं गुल्मार्शःकृमिमेहनुत् ||
Dhanwantri Nighantu Guduchyadi Varga- 29- 31
Properties and actions
निम्बो नियमनो नेता पिचुमन्दः सुतिक्तकः |
अरिष्टः सर्वतोभद्रः प्रभद्रः पारिभद्रकः ||
निम्बस्तिक्तरसः शीतो लघुः श्लेष्मास्रपित्तनुत् |
कुष्ठकण्डूव्रणान्हन्ति लेपाहारादिशीतलः ||
अपक्वं पाचयेच्छोफं व्रणं पक्वं विशोधयेत् ||
Kaiydeva Nighantu Aushadhi Varga- 879- 885
निम्बो नियमनोऽरिष्टः पिचुमन्दः सुतिक्तकः |
सुभद्रः सर्वतोभद्रः प्रभद्रः पारिभद्रकः ||
कृमिघ्नश्छर्दनो नेता यवनेष्टः शुकप्रियः |
निम्बस्तिक्तः कटुः पाके लघुः शीतोऽग्निवातकृत् ||
ग्राह्यहृद्यो जयेत् पित्तकफमेहज्वरकृमीन् |
कुष्ठकासारुचिश्वासहृल्लासश्वयथुव्रणान् ||
ग्राहि प्रवालं निम्बस्य रक्तपित्तकफकृमीन् |
कुष्ठघ्नं वातजननं नेत्ररोगान् विनाशयेत् ||
तद्वत् पत्राणि निम्बस्य व्रणघ्नानि विशेषतः |
शलाका निम्बपत्रस्य कासश्वासविनशिनी ||
कृमिघ्ना तु वरिष्ठा स्यात् कुष्ठज्वरविनाशिनी |
चक्षुष्यं निम्बपुष्पञ्च कृमिपित्तविषप्रणुत् ||
वातलं कटुपाकं स्यात् सर्वारोचकनाशनम् |
फलं तिक्तं रसे पाके कटुकं भेदनं लघु ||
अरूक्षमुष्णं कुष्ठघ्नं गुल्मार्शःकृमिमेहनुत् |
निम्बस्य पक्वं मधुरं सतिक्तं स्निग्धं फलं शोणितपित्तरोगे |
कफे प्रशस्तं नयनामयघ्नं, क्षतक्षयघ्नं गुरु पिच्छिलञ्च ||
निम्बबीजस्य मज्जा च कृमिकुष्ठविशोधनः ||
Raja Nighantu Prabhdradi Varga, 10- 13
अथ निगदितः प्रभद्रः पिचुमन्दः पारिभद्रको निम्बः |
काकफलः कीरेष्टो नेताऽरिष्टश्च सर्वतोभद्रः ||
धमनो विशीर्णपर्णी पवनेष्टः पीतसारकः शीतः |
वरतिक्तोऽरिष्टफलो ज्येष्ठामालकश्च हिङ्गुनिर्यासः ||
छर्दनश्चाग्निधमनो ज्ञेया नाम्नान्तु विंशतिः ||
प्रभद्रकः प्रभवति शीततिक्तकः कफव्रणक्रिमिवमिशोफशान्तये |
बलासभिद्बहुविषपित्तदोषजिद्विशेषतो हृदयविदाहशान्तिकृत् ||
Raja Nighantu Prabhdradi Varga, 14- 15
Nepal Nimba
नेपालनिम्बो नैपालस्तृणनिम्बो ज्वरान्तकः |
नाडीतिक्तोऽर्धतिक्तश्च निद्रारिः सन्निपातहा ||
नेपालनिम्बः शीतोष्णो योगवाही लघुस्तथा |
तिक्तोऽतिकफपित्तास्रशोफतृष्णाज्वरापहः ||
Priya Nighantu Haritkyadi varga, 180- 181
निम्ब: शीतो लघु स तिक्त: कफ पित्त ज्वरापह: |
कुष्ठा कृमि विषघ्न मेहघनो रक्त शोधन: |
वर्णे विदाहे पित्तस्य रक्तस्य परम औषधि |
निम्बस्य तैल॑ प्रकृतिस्थमेव नस्तो निषिक्त विधिना यथावत् |
मासेन गोक्षीरभुजो नरस्य यथाग्रभूत पलितं निहन्ति ||
Chakra Dutta, Trishna Chikitsa, 16- 10
तृषाचिकित्सायां निम्बप्रसवरस:
हित॑ भवेच्छर्दनमेव चात्र तप्तेन निम्बप्रसवोदकेन |
Bhava Parkasha, Chikitsa, 47- 69
व्रणेषु कृमिनाशनार्थम्
लेपो हिंगु निम्बकृतो अथवा |
Chakra Dutta, 55- 10
वाल्मीक रोगे निम्बतैलम् |
Shodhala
योनि दृदेकरणार्थम
प्रक्षालितम तु बहुशः पिचुमन्दतोयै: निम्बत्वचा तदनुनिर्मित: धूपकार्यम् |
स्त्रीणां नितम्बकुहरं प्रविमुक्तगन्ध॑ पैच्छिल्यदोषरहित॑ च भवेत् प्रगाढम् ||
Shodhala, Gada Nigraha, 2- 36- 87
कुष्ठे
य: खादेदभयारिष्टे अरिष्टामलके तथा |
स जयेत्सर्व कुष्ठ्न्तु मासाद ऊर्ध्वं न संशय: ||
Shodhala
गण्डमालायाम्
….तैलेन वारिष्टभवं…..नस्यम् |
Shodhala
रसायने
निम्बस्य तैल॑ प्रकृतिस्थमेव नस्ये निषिक्त॑ मधुना यथावत् |
मासेन गोक्षीरभुजो नरस्य जराग्रदूत॑ पत्त॑ निहिन्ति ||
Shodhala
कुष्ठ
यो निम्बपत्रशतमत्ति जलेन पिष्टम्
पिष्टान्नभुक् समयमेकमृतुत्रयं ना |
कुष्ठानि तस्य विषमानि चिरोत्थितानि
सिंहोद्धते मृगगणा: इव यान्ति नाशम् ||
Harita Samhita, Chikitsa, 35
व्रणशोधनार्थम
निम्बपत्राणि सम्पिष्य मधुना व्रणशोधनम् |
Harita Samhita, Chikitsa, 3- 46- 14
दन्तरोगे3- 56- 11
क्वाथश्च निम्बमूलस्य दन्तरोगनिवारण: |
Harita Samhita, Chikitsa,
विषप्रतिकारे
निम्बफलानि च |
उष्णोदकेन पीतानि जयेयुः तत्क्षणाद्विषम |
Chakra Dutta Amla Pitta, 52/ 28- 29
वात रक्त
पटोलनिम्बपत्राणि क्वथित्वा मधुसंयुतम् |
पाचनं वातरक्तानां तथा च शमनानि च ||
कांजीकें च सम्पिष्य पिचुमर्ददलानि च |
पित्त कफ जनित शूल सहित तीव्राम्लपित्ते पंञ्च निम्ब शक्तुयोगः
एको अशा: पश्चनिम्बनां द्विगुणो वृद्धदारुक: |
शक्तुर्दशगुणो देय: शर्करामधुरीकृत: ||
शीतेन वारिणा, पीतः शूलं पित्तकफोत्थितम् |
निहन्ति चूर्ण सक्षौद्रमम्लपित्तें सुदारुणम् ||
Harita Samhita, Chikitsa, 44- 28
लेपनं शस्यते तस्य वात रक्त प्रशांतये ||
दूषित व्रण शोधनार्थ निम्ब पत्रादि– शोधन केसरी लेपः
निम्बपत्र॑ तिला दन्ती त्रिवृत्सैन्धवमाक्षिकम् |
दुष्ठ व्रण प्रशमनो लेप: शोधनकेसरी ||
Vrinda Madhava, 57- 92, Chakra Dutta, Kshudra Roga Chikitsa, 55- 123
पलिते निम्बतैलनस्यम्
निम्बस्य बीजानि हि भावितानि भृङ्गस्य तोयेन तथा अशनस्य |
तैलन्तु तेषां विनिहन्ति नस्यादुग्धान्नभोक्तु: पलित॑ समूलम् ||
Raja Martanda
सुखप्रसवार्थम
कट्या बद्ध॑ योषितां सत्प्रसूतिं
कूर्यान्मूलं, निम्बवृक्षोद्धवं वा ||
Vanga Sena
शिशोः ज्वरे
निम्बस्य पत्रं माक्षिक सर्पियुक्तन्तु धूपनम् |
ज्वरवेगं निहन्त्याशु बालानान्तु विशेषतः ||
Sharangdhara Samhita, 2- 9- 152
पालित्ये
निम्बबीजतैलम्
Sharangdhara Samhita, 3- 13- 29, Vanga Sena
नेत्ररोगे
शुण्ठी निम्बदलै: पिण्ड: सुखोष्ण: स्वल्पसैन्धव: |
धार्याश्च क्षुषि सङ्क्शेपो शोथे कण्डूव्यथापह: ||
Vanga Sena, Hrida Roga, 26
कफज हद्रोगे
निम्बकोषातकीभ्यां वाम्य॑ हदि कफो उत्तिठे |
Siddha Bhaishjya Manimala, 4- 5- 38
मूत्रकृच्छे
निम्बशरी: सड्कषुण्णा मृत्पात्रै: सायमप्सु विनिमग्रा: |
प्रातस्ता: पुनराप: पित्त प्रकृच्छमपहन्यु: ||
Chakra Dutta
कामलायाम
….निम्बस्य वा रस: |
प्रातर्माक्षिकसंयुक्त: शीलित: कामलापह: ||
Vrinda Madhava, 52- 8, Chakra Dutta, Udard Kotha Sheeta Pitta, 50- 9
उदर्द- कोठादौ
निम्बस्य पत्राणि सदा घृतेन |
धात्रीविमिश्रान्यथवोपयुज्यात् ||
विस्फोटकोठ क्षत शीत पित्त–कण्ड्वस्त्रपित्तं सहसा च हन्यात् (जह्मात्) |
Bhava Parkasha, Chikitsa, 7- 24
क्रिमिषु
निम्ब पत्र समुद्धूतं रसं क्षौद्रयुतं पिबेत् |
Chakra Dutta, 47- 6
पित्त –रक्तजो उपदंश चिकित्सायां निम्बादि चूर्णम्
Bhava Parkasha Chikitsa, 9- 98
रक्तपित्ते
पटोल निम्ब वेत्राग्र प्लक्ष वेतस पल्लवा: |
शाकार्थ शाकसात्म्यानां हिता: ||
Bhava Parkasha, Kshudra Roga Adhikara, 54/ 63- 64
कुष्ठ रोग चिकित्सायां पश्चनिम्बकावलेहम्
Charaka Samhita Chikitsa, 7
कुष्ठ
….निम्ब पटोलस्य….. |
इति षट् कषायोष्णा: कुष्ठ्घ्ना निर्दिष्टा:….|
…..स्त्राने पाने च मता: |
Sushruta Samhita, Uttara Tantra, 39/ 282
दाहज्वर
मधु फाणित॑ युक्तेन निम्ब पत्राम्भसा अपि वा |
दाहज्वरात्त॑ मतिमान् वामयेत् क्षिप्रमेव च ||
Sushruta Samhita, Uttara Tantra, 48
कफज तृष्णायाम्
हित॑ भवेच्छ्दनमेव चात्रे तपतेन निम्ब प्रसादोदकेन |
Sushruta Samhita, Chikitsa Sthana, 11- 9
सुरामेह
सुरामेहिनं निम्बकषायम् |
Sushruta Samhita, Chikitsa Sthana, 20/ 27
पदमिनी कण्टके वमनार्थ निम्बोदकम्
निम्बोदकेन वमनं पद्मिनीकण्टके हितम् ||
निम्बोदककृतं सर्पि: सक्षौद्रं पानमिष्यते ||
अरुंषिकायाम्
अरुंषिकाहते रक्ते सेचयन्रिम्बवारिणा |
Sushruta Samhita, Chikitsa Sthana, 9
जातसत्त्वे कुष्ठे
….निम्बक्काथ॑ जातसत्त्व: पिबेद्वा |
Sushruta Samhita, Chikitsa Sthana, 20
पद्मिनीकण्टके
निम्बारग्वधयो: क्वाथो हित उत्सादने भवेत् |
Ashtanga Hridya, Uttara Tantra, 24- 34
खालित्ये पालित्ये च
मास वा निम्बज तैल॑ क्षीरभुक् नावयेद् यति: |
Charaka Samhita, Chikitsa Sthana, 7- 158
कुष्ठे निम्ब क्वाथस्य बहुविधप्रयोगा:
….निम्बखदिरश्च |
स्नाने पाने लेपे क्रिमिकुष्ठनुत् सगोमूत्र: |
Charaka Samhita Chikitsa Sthana, 30/ 99
कफजप्रदरे
मद्यै्निम्बगुडूच्यौ वा कफजे असृग्दरे पिबेत् |
Chakra Dutta Netra Roga Chikitsa, 59/ 35
नेत्र प्रकोप शम्नाय निम्ब पत्र गुटिका प्रयोग
पिष्टे निम्बस्य पत्रैरतिविमलतंरै जाति सिन्धूत्थमिश्रा
अन्तर्ग्भ दधाना पटुतर गुटिका पिष्टलोध्रेन भृष्टा |
तूलै: सौवीर सान्द्रै रतिशयमृदुभिर्वेष्टिता सा समन्ता–
च्यक्षुकोपप्रशान्तिं चिरमुपरि दृशोशभ्रम्यमाणा करोति ||
Chakra Dutta Unmada Chikitsa, 20/ 48
उन्मादे निम्बादि धूप:
Charaka Samhita Chikitsa Sthana, 7/ 157
उग्र गलित कुष्ठ
प्रपतन्तु लसीका प्रस्तुतेषु गात्रेषु जन्तुजग्धेषु |
मूत्र॑ निम्बं विडंगे स्नानं पान प्रदेहश्च |
Chakra Dutta, 50/ 74- 83
सर्व कुष्ठ पंञ्च निम्बचूर्णम्
Charaka Samhita, Chikitsa Sthana, 1/ 135, Chakra Dutta, Kustha Chikitsa, 50/ 93- 97
कुष्ठ निम्बघृतम्
….निम्बघृतं…. |
कुष्ठेषु रक्तपित्त प्रबलेषु भिषग्जितं सिद्धम् ||
कुष्ठादया: चिकित्सार्थ तिक्तषट्पलकं घृतम् |
Charaka Samhita Chikitsa Sthana, 221
रक्त अर्श प्रतिसारणम्
…निम्बघृताभ्यां…..|
दाहे कलेदे च गुद्रभंशे गुदजा: प्रतिसारंणीया: स्यु: ||
Charaka Samhita Chikitsa Sthana, 16/ 63
कामलायां प्रात: कालिकयोगम्
….निम्बस्य वा रसम् |
शीत मधुयुतं प्रात: कामला अर्त पिबेन्नर: ||
Sharangdhara Samhita, 2- 5- 5, Bhava Parkasha, Vrana Shotha Adhikara, 47/ 60
व्रण शोधनरोपणार्थे
लेपान्रिम्बदलै: कल्को व्रणशो धनरोपण: |
भक्षणाच्छ्दि मन्दाग्नि पित्तमेष्मकृमीन्हरेत् ( कृमीन् जयेतू ) ||
व्रण निम्बदले वर्त्या सूक्ष्मान् हि सन्धिमर्मजान् ||
Bhava Parkasha, Madhyama Khanda, 47/ 70
व्रणे निबादि धूपनम्
निम्ब पत्र वर्ची हिंगु सर्पिरलवणसर्षपै: |
धूपनं स्याद् व्रणे रूक्ष कृमि कण्डू रुजा अपहम् ||
Bhava Parkasha, Kshudra Roga Adhikara, 141- 142
पदमिनीकण्टके निम्बादिघृतम्
चतुर्गुणेन निम्बोत्थपत्रक्काथेन गोघृतम्
पचेत्ततस्तु, निम्बस्य कृतमालस्य पत्रजै: ||
कल्कैर्भूय: पचेत्सिद्ध॑तत्पिबेत्पलसम्मितम् |
पद्मिनी कण्टकाद्रोगान्मुक्तो भबति नान्यथा ||
Bhava Parkasha, Yoni Roga Adhikara, 70- 42
योनि ( पूययुक्त ) रोगे योनि शोधनार्थम्
योन्यां तु पूयस्राविण्यां शोधनद्रव्यनिर्मितैः |
सगोमूत्रै: सलवणै: पिण्डै: सम्पूरण हितम् ||
Chakra Dutta, 44- 35
व्रण शोधन रोपणार्थ निम्बपत्रादिवर्त्ति:
निम्ब पत्र घृत क्षौद्र दार्वी मधुक संयुतता |
वर्त्तिस्तिलानां कल्को वा शोधयेद्रोपयेत् व्रणान् ||
Chakra Dutta, 50- 64, Shodhala, 2- 36- 37
कुष्ठ उपचारार्थ निम्बपत्रासेवनम्:
य: खादेदभया अरिष्टमरिष्टमालकानि वा |
स जयेत् सर्वकुष्ठानि मासा ऊर्ध्वं न संशय: ||
Gada Nigreha, 6- 9- 14
योनिविकारे
प्रक्षालित॑ तु बहुश: पिचुमन्दतोयै: निम्ब त्वचा तदनुनिर्मित धूपकार्यम् |
ख्रीणां नितम्बकुहर प्रविमुक्तगन्ध॑ पैच्छिल्यदोषरहितञ्च भवेत् प्रगाढम ||
Vrinda Madhava, 68- 2
विष प्रतिषेधे
मयूर॑ निम्बपत्राभ्यां खादे मेषगते रवौ |
अब्दमेकं न भीति: स्याद् विषार्तस्य न संशय: ||
Charaka Samhita Chikitsa Sthana, 30/ 259
स्तन्यशोधने
निम्ब वेत्राग्कुलक वार्ताकामलकै: श्रितान |
स व्योष सैन्धवान् यूषान् दापयेत् स्तन्यशोधनम् ||
Sharangdhara Samhita, 3- 13- 35
नेत्ररोगे निम्ब
लौहस्य पात्रे संघृष्टो रसो निम्बफलोद्धव: |
किंच्चिद घनो बहिलेपानरेत्रबाधां व्यपोहति ||
Vanga Sena Netra Roga, 117
निम्बपत्रै: कृत चूर्ण लोध्र चूर्ण समन्वितम् |
वस्त्र बद्ध जले क्षिप्त॑ पूरणं नेत्ररोगनुत् ||
Charaka Samhita Chikitsa Sthana, 25- 84
व्रण
निम्ब कोलक पत्राणि कषाया: शोधना मता: |
Sushruta Samhita, Chikitsa Sthana, 1/ 68
निम्ब पत्र मधुभ्यां तु युक्त: संशोधन: स्मृत: |
पूर्वाभ्यां सर्पिषा चापि युक्त श्च आप्य रोपण: ||
Vrinda Madhava, 44/ 28
पूर्वाभ्यां सर्पिषा चापि युक्तश्राप्युपरोपण: |
निम्बपत्रतिलै: कलको मधुना व्रण शोधन: |
रोपणः सर्पिषा युक्तो यवकल्के अप्ययं विधि: ||
Vrinda Madhava, 57/ 20
पदमिनीकण्टके
“निम्बोदककृतं सर्पि: सक्षौद्रं पानमिष्यते ।
Sushruta Samhita Chikitsa Sthana, 20, Ashtanga Sangreha, Uttara Tantra, 37/ 6, Vrinda Madhava, 57/ 20
निम्बारग्वधयो: कल्को हित उत्सादने भवेत् |
Sharangdhara Samhita, 3- 52- 53
त्वक रोग
धतूर निम्ब ताम्बली पत्राणां स्वरसै: पृथक |
अस्य प्रलेप मात्रेण पामाद्रद्रूविचर्चिका: ||
कण्डूश्च रकस श्चैव प्रशमं यान्ति वेगत: ||
Charaka Samhita Chikitsa Sthana, 14/ 160
दाहे
बदरी पल्लवोत्थश्च तथैवारिष्ठकोद्धव: |
फेनिलायाश्य य: फेनस्तैर्दाहलेपनं शुभम् ||
Vaidya Jeevanam, 1/ 28
तृड्दाह मोहा: प्रशमं प्रयान्ति
निम्ब प्रवालोत्थित फेन लेपात् |
Vrinda Madhava, 53/ 18/ 19
अम्ल पित्ते:
एको अस: पञ्च निम्बानाम द्विगुणो वृद्धदारुक: |
सक्तुर्दशगुणो देय: शर्करामधुरीकृत: ||
शीतेन वारिणा पीत॑ शूलं पित्तकफोदभवम् |
निहन्ति चूर्ण सक्षौद्रमम्लपित्त॑: सुदुस्तरम् ||
Kashyapa Samhita, page 344
शोथे
निम्बाह्लोटोरुबुकानां तंकार्या: कुटजस्य च |
नक्तमालस्य वैशम्य पत्रक्कनाथो अवगाहन: ||
Gada Nigreha, 2- 36- 99
कुष्ठ
यो निम्ब पत्र शतमत्ति जलेन पिष्ट॑ पिष्टान भुक समयमेकमूतुत्रयं वा |
कुष्ठानि तस्य विषमानि सिंहोद्धते मृगगणा इव यान्ति नाशम् ||
Vrinda Madhava, 51/ 60- 68
पंञ्च निम्बचूर्णम |
Siddha Bhaishjya Manimala, 4- 238
रक्तार्शासि
मूलकमुत्कोर्य महत्तत्र पिधाय पिचुमन्दमज्ञानम् |
पुटपाक रीति पक्वं पिष्टा गुटिकीकृतं निहन्त्यर्श: ||
Kashyapa Samhita, page 171
ज्वर
धृत॑ निम्बस्य पत्राणि मूल पुष्प॑ फल त्वचम् |
अरिष्टो नाम धूपो अयं अरिष्टं कुरुते क्षणात् ||
Specific Formulation of Nimba
Nimba can be considered a Kalpa Vriksha as every part of it is very useful. Charaka opines that one who uses parts of Nimba to take a bath, in food, and for preparing a bed to sleep for a year will never suffer from skin diseases.
- Nimba Churna for Kustha, Vata Rakta
- Nimba Amritadi Kshaya for Visphota
- Nimbadi Kwatha for Kaphaja Jwara, Pitta Sotha
- Pancha Nimba Churna for Visarpa and Sarva Kustha
- Tiktka Ghrita for Kustha, Visarpa
- Panch Tikta Ghrita Guggulu for Parmeha, Kustha
Contraindications and Side Effects of Nimba
- Sometimes use of Nimba may result in loose stools, decreased fertility, seizures in children, acidosis, vomiting, etc.
- Avoid the use of Nimba in people who are trying to conceive, pregnant, and lactating mothers.
- Avoid the use of Nimba if you are suffering from stomach illness, Kidney, and liver issues.
Suggestive Reading Regarding Azadirachta indica
- Satyanarayana K, Sravanthi K, Shaker IA, Ponnulakshmi R. Molecular approach to identify antidiabetic potential of Azadirachta indica. J Ayurveda Integr Med. 2015 Jul- Sep, 6 (3): 165- 74. Doi: 10. 4103/ 0975- 9476.157950. PMID: 26604551; PMCID: PMC 4630690.
- Pedroza, David & Benjamin, Serrano-Gallardo & Edith, Escobar- Avila & Delia, Alma & Nava- Hernandez, & Patricia, Martha & Maria, Vega-Menchaca & Carmen, Del. (2017). HIV-1 infection inhibition by neem (Azadirachta indica A. Juss.) leaf extracts and Azadirachtin. Indian journal of traditional knowledge. 16. 437- 441.
- Dhama, Ankit & Ahmad, Shamim & Kumar, Praveen & Paharia, Ashish. (2020). Evaluation of Antidiarrhoeal Potential of Azadirachta Indica Stem Bark Extract in Rats. International Journal of Scientific and Research Publications (IJSRP). 10. p9913. 10. 29322/ IJSRP. 10. 03. 2020. p9913.
- Awah, Francis & Uzoegwu, Peter & Ifeonu, Patrick. (2011). In vitro anti- HIV and immunomodulatory potentials of Azadirachta indica (Meliaceae) leaf extract. African Journal of Pharmacy and Pharmacology. 5. 1353- 1359.
- Bharat, Pokhrel & Sagar, Rijal & Sulav, Raut & Pandeya, Ankit & eya. (2015). Investigations of antioxidant and antibacterial activity of leaf extracts of Azadirachta indica. African Journal of Biotechnology. 14. 3159- 3163. 10. 5897/ AJB2015. 14811.
- Mankala, Dr. Santhosh Kumar. (2011). In vivo Antidiabetic evaluation of Neem leaf extract in alloxan-induced rats. Journal of Applied Pharmaceutical Science. 1. 100-105.
- Baghel, Shalu & Singh, Charanjeet. (2019). ANTIHYPERLIPIDEMIC ACTIVITY OF METHANOLIC EXTRACT OF AZADIRACHTA INDICA. Journal of Biomedical and Pharmaceutical Research. 8. 10. 32553/ jbpr. v8i6. 678.
- Khan, Shaista. (2015). In Vitro Analysis of Antiallergic Activity of Neem (Azadirachta Indica) for Reduction of Wheat Allergens. Sindh Univ. Res. Jour. (Sci. Ser..). 47. 485- 488.
- Satyanarayana, K & Sravanthi, K & Shaker, I., Anand, & Ponnulakshmi, R. (2015). Molecular approach to identify antidiabetic potential of Azadirachta indica (neem) on the expression insulin signaling molecules and glucose oxidation in skeletal muscle of high-fat and fructose- induced type- 2 diabetic adult male rat. Journal of Ayurveda and Integrative Medicine. 10. 4103/ 0975- 9476. 157950.
- Chattopadhyay, Rabiranjan. (2004). Possible mechanism of hepatoprotective activity of Azadirachta indica leaf extract: Part II. Journal of Ethnopharmacology. 89. 217- 9. 10. 1016/ j. jep. 2003. 08. 006.
- Thakurta, Prarthana & DeBhowmik, Poulami & Mukherjee, Souryadeep & Hajra, Tapas & Patra, Amarendra & Bag, Prasanta K. (2007). Antibacterial, antisecretory, and antihemorrhagic activity of Azadirachta indica is used to treat cholera and diarrhea in India. Journal of Ethnopharmacology. 111. 607- 12. 10. 1016/ j. jep. 2007. 01. 022.
- Maruthappan, K. (2009). Hepatoprotective effect of Azadirachta indica (Neem) leaves against alcohol induced liver injury in albino rats. Journal of Pharmacy Research.
- Shahbaz, Benish & Akhtar, Shabana & Muddassir, Maria & Yasmin, Shagufta & Akram, Ayesha & Majeed, Muhammad & Ahmad, Mukhtiar & Shafiq, Muhammad & Arshad, Shafia & Hadi, Faheem & Tahir Maqbool, Dr & Hayat, Sikander & Muhammad, Tahir. (2023). Anti-diabetic activity of a novel Phytoformulation of Tribulus terrestris, Prunus dulcis, Cicer arietinum, and Azadirachta indica in streptozotocin-induced diabetic rats. 19. 360- 373.
- Baligar, Nagappa & Aladakatti, Ravindranath & Ahmed, Mukhtar & Hiremath, Murigendra. (2014). Hepatoprotective activity of the neem-based constituent azadirachtin-A in carbon tetrachloride intoxicated Wistar rats. Canadian journal of physiology and pharmacology. 92. 267- 77. 10. 1139/ cjpp- 2013- 0449.
- Thiagarajan, Kalaivani & Meignanam, E. & Premkumar, N. & Siva, Ramamoorthy & Vijayakumar, Vijayaparthasarathi & Chandrasekaran, Rajasekaran & Subramanian, Ramya & Jayakumararaj, R. (2009). Studies on Hepatoprotective Properties of Leaf Extracts of Azadirachta indica A. Juss (Meliaceae). Ethnobotanical Leaflets. 13. 165- 170.
- Nahak, Dr. Gayatri & Sahu, Rajani. (2010). Antioxidant activity in bark and roots of Neem (Azadirachta indica) and Mahaneem (Melia azedarach). Continental J. Pharmaceutical Sciences. 4. 28- 34.
- Nagesh, Simhadri & M, Muniappan & I, Kannan & Subramanian, Viswanathan. (2018). ANTIFUNGAL ACTIVITY OF A SECONDARY METABOLITE OF AZADIRACHTA INDICA AND ITS DERIVATIVES – AN IN-SILICO STUDY. Asian Journal of Pharmaceutical and Clinical Research. 11. 175. 10. 22159/ ajpcr. 2017. v11i1. 22171.
- Kumar, B Dinesh & Mitra, Analava & Mahadevappa, Manjunatha. (2011). Azadirachtolide: An anti-diabetic and hypolipidemic effect from Azadirachta indica leaves. Pharmacognosy Communications. 1. 78- 84. 10. 5530/ pc. 2011. 1. 5.
- Senthuri, N & Somasundaram, Ambiga. (2022). IN VITRO ANTI-DIABETIC AND ANTIOXIDANT ACTIVITIES OF Azadirachta indica AND Aloe vera FORMULATION.
- Patil, Prabhakar & Patil, Sudha & Mane, Abhay & Verma, Sushilkumar. (2013). Antidiabetic activity of alcoholic extract of Neem Azadirachta Indica root bark. National Journal of Physiology, Pharmacy and Pharmacology. 3. 142- 146. 10. 5455/ njppp. 2013. 3. 134- 138.
- Sharma, Shubham & Chaurasia, Lovely & Tyagi, Sunayana. (2022). Therapeutic activity study in fungal disease by Azadirachta indica. Biomedical Research. 33. 119.
- Mostofa, Mahbub & Choudhury, Mohammed & Hossain, Md.Monir & Islam, Md & Islam, Muh & Sumon, Md Mahmudul Hasan. (2008). Antidiabetic effects of Catharanthus roseus, Azadirachta indica, Allium sativum, and glimepiride in experimentally diabetic induced rats. Bangladesh Journal of Veterinary Medicine. 5. 10. 3329/ bjvm. v5i1. 1324.
- Kumar, Sanjay & Vandana, Udaya & Agrawal, divya & Hansa, Jagadish. (2015). Analgesic, Anti-inflammatory, and Anti-Pyretic Effects of Azadirachta indica (Neem) Leaf Extract in Albino Rats. International Journal of Science and Research (IJSR). 4. 713- 721.
- Adekunle, Adewuyi & Adelusi, Temitope & Kamdem, Dr. Jean Paul & Ishmael, A & Akintade, B. (2016). Insulinomimetic, Antihyperlipidemic, and Antioxidative Properties of Azadirachta indica. Possible Mechanism of Action. British Journal of Medicine and Medical Research. 17. 1- 11. 10. 9734/ BJMMR/ 2016/ 26897.
- Chattopadhyay, Rabiranjan & Bandyopadhyay, M. (2006). Effect of Azadirachta indica leaf extract on serum lipid profile changes in normal and streptozotocin-induced diabetic rats. African Journal of Biomedical Research. 8. 10. 4314/ ajbr. v8i2. 35769.
- Basha, Saleem & Baruah, Mriganka & Shaker, A. & Kondaveeti, Dr.Suresh & Narayana, S. (2012). Hypoglycemic and hypolipidemic effect of Azadirachta indica seed oil and mehani (polyherbal formulation) on alloxan-induced diabetic albino rats. Research Journal of Pharmaceutical, Biological and Chemical Sciences. 3. 239- 246.
- Prabagar, Subramaniam & Nandakumar, Jeyarani & Prabagar, Jasotha & Thuraisingam, Suganja. (2020). SPC Journal of Plant Sciences Antimicrobial activity of Azadirachta Indica (neem) leaves and stem bark aqueous extracts.
- Sadasivam, Poompavai & Sree, v.gowri & RamSugitha, B.. (2021). Enhanced Extraction and Improved Anticancer Activity of Neem ( Azadirachta indica ) Leaves by Electroporation Technique. IETE Journal of Research. 1- 11. 10. 1080/ 03772063. 2021. 1962743.
- SALAZAR, Daniel & Hoyos, Rodrigo & Orozco-Sánchez, Fernando & Arango, Myrtha & Gomez Londoño, Luisa. (2015). Antifungal activity of neem (Azadirachta indica: Meliaceae) extracts against dermatophytes. Acta Biologica Colombiana. 20. 201- 207. 10. 15446/ abc. v20n3. 45225.
- Paul, Rajkumar & Prasad, Murari & Sah, Nand. (2011). Anticancer biology of Azadirachta indica L (Neem): A mini review.. Cancer biology & therapy. 12. 467-76. 10. 4161/ cbt. 12. 6. 16850.
- Khan, Mohsin & Yaqoob, Shadma & Ahmad, Sharique. (2021). Antimicrobial Activity of Azadirachta indica, against Target Pathogens and Its Utility as a Disinfectant and Floor Cleaner. Journal of Evolution of Medical and Dental Sciences. 10. 1899- 1903. 10. 14260/ jemds/ 2021/ 392.
- Herrera Calderon, Oscar & Ejaz, Kainat & Wajid, Mahnoor & Shehzad, Muzzamil & Tinco-Jayo, Johnny & Enciso, Edwin & Franco-Quino, César & Yuli Posadas, Ricardo & Chumpitaz-Cerrate, Victor. (2019). Azadirachta indica: Antibacterial Activity of Neem Against Different Strains of Bacteria and their Active Constituents as Preventive in Various Diseases. Pharmacognosy Journal. 11. 1597- 1604. 10. 5530/ PJ. 2019. 11. 244.
- Adamu, Muhammad & Lawan, Ibrahim & Abubakar, Ahmed & Dangora, Ibrahim. (2019). Antimicrobial Activity of Azadirachta indica (Neem) Leaf Extract Against Some Clinical Isolates.
- Raut, Ranjit R. & Sawant, Ajit & Jamge, Bhagyshree. (2014). Antimicrobial activity of Azadirachta indica (Neem) against Pathogenic Microorganisms. Journal of Academia and Industrial Research. 3. 327- 329.
- Santra, Soumya & Naik, M.R. & Behera, R. & Agrawal, Divya & Kumar, Sanjay & Patnaik, S. (2014). Antipyretic effect of Azadirachta indica leaf extract (Neem Leaf Extract) on albino rats. Research Journal of Pharmaceutical, Biological and Chemical Sciences. 5. 669- 673.
- Alzohairy MA. Therapeutic Role of Azadirachta indica (Neem) and Its Active Constituents in Disease Prevention and Treatment. Evid Based Complement Alternat Med. 2016; 2016: 7382506. Doi: 10. 1155/ 2016/ 7382506. Epub 2016 Mar 1. PMID: 27034694; PMCID: PMC 4791507.
- Sarkar S, Singh RP, Bhattacharya G. Exploring the role of Azadirachta indica (neem) and its active compounds in the regulation of biological pathways: an update on molecular approach. 3 Biotech. 2021 Apr; 11 (4): 178. doi: 10. 1007/ s13205- 021- 02745- 4. Epub 2021 Mar 20. PMID: 33927969; PMCID: PMC- 7981372.
- Wylie MR, Merrell DS. The Antimicrobial Potential of the Neem Tree Azadirachta indica. Front Pharmacol. 2022 May 30; 13: 891535. doi: 10. 3389/ fphar. 2022. 891535. PMID: 35712721; PMCID: PMC- 9195866.
- Ali E, Islam MS, Hossen MI, Khatun MM, Islam MA. Extract of neem (Azadirachta indica) leaf exhibits bactericidal effect against multidrug-resistant pathogenic bacteria of poultry. Vet Med Sci. 2021 Sep; 7 (5):1921-1927. Doi: 10. 1002/ vms3. 511. Epub 2021 May 6. PMID: 33955693; PMCID: PMC- 8464248.
- Batra N, Kumar VE, Nambiar R, De Souza C, Yuen A, Le U, Verma R, Ghosh PM, Vinall RL. Exploring the therapeutic potential of Neem (Azadirachta Indica) for the treatment of prostate cancer: a literature review. Ann Transl Med. 2022 Jul; 10 (13): 754. Doi: 10. 21037/ atm- 22- 94. PMID: 35957716; PMCID: PMC- 9358515.
- Mistry KS, Sanghvi Z, Parmar G, Shah S. The antimicrobial activity of Azadirachta indica, Mimusops elengi, Tinospora cardifolia, Ocimum sanctum, and 2% chlorhexidine gluconate on common endodontic pathogens: An in vitro study. Eur J Dent. 2014 Apr; 8 (2): 172- 177. doi: 10. 4103/ 1305- 7456. 130591. PMID: 24966766; PMCID: PMC- 4054046.
- Yarmohammadi F, Mehri S, Najafi N, Salar Amoli S, Hosseinzadeh H. The protective effect of Azadirachta indica (neem) against metabolic syndrome: A review. Iran J Basic Med Sci. 2021 Mar; 24 (3): 280- 292. Doi: 10. 22038/ ijbms. 2021. 48965.11218. PMID: 33995939; PMCID: PMC- 8087850.
Suggestive Reading Regarding Millingtonia hortensis.
- Kumar, M. & Ravichandran, N. (2011). Cytotoxicity and antimicrobial studies of the stem bark of Millingtonia hortensis Linn. International Journal of Pharmacy and Pharmaceutical Sciences. 3. 247- 249.
- Tansuwanwong, Siwapong & Hiroyuki, Yamamoto & Imai, Kohzoh & Vinitketkumnuen, Usanee. (2006). Induction of apoptosis in RKO colon cancer cell line by an aqueous extract of Millingtonia hortensis. Asian Pacific journal of cancer prevention: APJCP. 7. 641- 4.
- Jayabharathi, M. & Chitra, Muthaiyan. (2011). Evaluation of anti-inflammatory, analgesic, and antipyretic activity of Moringa concanensis Nimmo. Journal of Chemical and Pharmaceutical Research. 3. 802- 806.
- Chaiyasit, Sittiwet. (2009). Antimicrobial Activities of Millingtonia hortensis Linn. Flowers Essential Oil. Journal of Pharmacology and Toxicology. 4. 41-44. 10. 3923/ jpt. 2009. 41. 44.
- Babitha, S & Banji, David, & Banji, Otilia. (2012). Antioxidant and hepatoprotective effects of flower extract of Millingtonia hortensis Linn. on carbon tetrachloride-induced hepatotoxicity. Journal of pharmacy & bioallied sciences. 4. 307- 12. 10. 4103/ 0975- 7406.
- Jumnongprakhon, Pichaya & Pinkaew, Decha & Phuneerub, Pravaree. (2021). The antiaging property of the aqueous extract of Millingtonia hortensis flowers in aging neurons. Journal of Advanced Pharmaceutical Technology & Research. 12. 14. 10. 4103/ japtr. JAPTR_ 187_ 20.
- Kumar, M. & Kavimani, S. (2014). Anthelmintic activity of Millingtonia hortensis Linn. F. stem bark on Indian adult earthworm. Der Pharmacia Lettre. 6. 89- 91.
- Tansuwanwong, Siwapong & Yamamoto, Hiroyuki & Imai, Kohzoh & Vinitketkumnuen, Usanee. (2007). ANTIPROLIFERATIVE EFFECT ON COLON CANCER CELL LINES BY AQUEOUS EXTRACT FROM THE BARK OF MILLINGTONIA HORTENSIS. 46.
- Kaushik, R. & Saini, Paarisha. (2008). Larvicidal activity of leaf extract of Millingtonia hortensis (Family: Bignoniaceae) against Anopheles stephensi, Culex quinquefasciatus, and Aedes aegypti. Journal of Vector-Borne Diseases. 45. 66- 9.
- Arumugam, Janaki & Muthu, Babu. (2017). Phytochemical screening, antioxidant and antibacterial activities of Millingtonia hortensis (L). International Journal of Current Pharmaceutical Review and Research.
- Chumbhale, Deshraj, & Chavan, & Upasani, Cd. (2017). PHENOLIC CONTENT AND IN VITRO ANTIOXIDANT ACTIVITY OF MILLINGTONIA HORTENSIS LINN. International Journal of Pharmaceutical, Chemical and Biological Sciences. 2017. 217- 222.
- Puri, S, & Sharma, P.D. (2007). Antifungal activity of Millingtonia hortensis. Indian Journal of Pharmaceutical Sciences. 69. 10. 4103/ 0250- 474X. 36959.
- Jetty, A. & Iyengar, D.S. (2000). Antimicrobial Activity of Millingtonia Hortensis Leaf Extract. Pharmaceutical Biology. 38. 157- 160. 10. 1076/ 1388- 0209% 28200004% 293821- 1FT157.
- Jumnongprakhon P, Pinkaew D, Phuneerub P. The antiaging property of the aqueous extract of Millingtonia hortensis flowers in aging neurons. J Adv Pharm Technol Res. 2021 Jan- Mar; 12 (1): 14- 21. doi: 10. 4103/ japtr. JAPTR_ 187_ 20. Epub 2021 Jan 9. PMID: 33532349; PMCID: PMC- 7832191.
- Babitha S, Banji D, Banji OJ. Antioxidant and hepatoprotective effects of the flower extract of Millingtonia hortensis Linn. on carbon tetrachloride-induced hepatotoxicity. J Pharm Bioallied Sci. 2012 Oct; 4 (4): 307- 12. doi: 10. 4103/ 0975- 7406. 103258. PMID: 23248564; PMCID: PMC- 3523526.
- Rengasamy KRR, Mahomoodally MF, Joaheer T, Zhang Y. A Systematic Review of Traditionally Used Herbs and Animal-Derived Products as Potential Analgesics. Curr Neuropharmacol. 2021; 19 (4): 553- 588. doi: 10. 2174/ 1570159- X18666- 200808151522. PMID: 32781962; PMCID: PMC- 8206464.
- Patel K, Patel DK. Medicinal importance, pharmacological activities, and analytical aspects of hispidulin: A concise report. J Tradit Complement Med. 2016 Dec 10; 7 (3): 360- 366. Doi: 10. 1016/ j. jtcme. 2016. 11. 003. PMID: 28725632; PMCID: PMC- 5506639.
- Tor-Ngern P, Leksungnoen N. Investigating carbon dioxide absorption by urban trees in a new park of Bangkok, Thailand. BMC Ecol. 2020 Apr 13; 20 (1): 20. doi: 10. 1186/ s12898- 020- 00289- 4. PMID: 32284054; PMCID: PMC- 7155315.
- Elkington BG, Sydara K, Newsome A, Hwang CH, Lankin DC, Simmler C, Napolitano JG, Ree R, Graham JG, Gyllenhaal C, Bouamanivong S, Souliya O, Pauli GF, Franzblau SG, Soejarto DD. New finding of an anti-TB compound in the genus Marsypopetalum (Annonaceae) from a traditional herbal remedy of Laos. J Ethnopharmacol. 2014 Feb 3; 151 (2): 903- 11. doi: 10. 1016/ j. jep. 2013. 11. 057. Epub 2013 Dec 11. PMID: 24333958; PMCID: PMC- 3933013.
- Bhattacharya R, Saha S, Kostina O, Muravnik L, Mitra A. Replacing critical point drying with a low-cost chemical drying provides comparable surface image quality of glandular trichomes from leaves of Millingtonia hortensis L. f. in scanning electron micrograph. Appl Microsc. 2020 Jul 17; 50 (1): 15. Doi: 10. 1186/ s42649- 020- 00035- 6. PMID: 33580468; PMCID: PMC- 7818294.
- Paibon W, Yimnoi CA, Tembab N, Boonlue W, Jampachaisri K, Nuengchamnong N, Waranuch N, Ingkaninan K. Comparison and evaluation of volatile oils from three different extraction methods for some Thai fragrant flowers. Int J Cosmet Sci. 2011 Apr; 33 (2): 150-6. doi: 10. 1111/ j. 1468- 2494. 2010. 00603. x. PMID: 20704598.
- Tag H, Kalita P, Dwivedi P, Das AK, Namsa ND. Herbal medicines used in the treatment of diabetes mellitus in Arunachal Himalaya, northeast India. J Ethnopharmacol. 2012 Jun 14; 141 (3): 786- 95. doi: 10. 1016/ j. jep. 2012. 03. 007. Epub 2012 Mar 13. PMID: 22433536.
- Yousefbeyk F, Vatandoost H, Golfakhrabadi F, Mirzaee Z, Abai MR, Amin G, Khanavi M. Antioxidant and Larvicidal Activity of Aerial Parts of Scrophularia striata against Malaria Vector Anopheles stephensi. J Arthropod Borne Dis. 2018 Jun 13; 12 (2): 119- 126. PMID: 30123805; PMCID: PMC- 6091803.
- Salehi B, Ata A, V Anil Kumar N, Sharopov F, Ramírez-Alarcón K, Ruiz-Ortega A, Abdulmajid Ayatollahi S, Tsouh Fokou PV, Kobarfard F, Amiruddin Zakaria Z, Iriti M, Taheri Y, Martorell M, Sureda A, Setzer WN, Durazzo A, Lucarini M, Santini A, Capasso R, Ostrander EA; Atta-ur-Rahman; Choudhary MI, Cho WC, Sharifi-Rad J. Antidiabetic Potential of Medicinal Plants and Their Active Components. Biomolecules. 2019 Sep 30; 9 (10): 551. doi: 10. 3390/ biom- 9100551. PMID: 31575072; PMCID: PMC- 6843349.
- Benvenuti S, Mazzoncini M. The Biodiversity of Edible Flowers: Discovering New Tastes and New Health Benefits. Front Plant Sci. 2021 Feb 22; 11: 569499. doi: 10. 3389/ fpls. 2020. 569499. PMID: 33692813; PMCID: PMC- 7937964.
- Rashid HM, Mahmod AI, Afifi FU, Talib WH. Antioxidant and Antiproliferation Activities of Lemon Verbena (Aloysia citrodora): An In Vitro and In Vivo Study. Plants (Basel). 2022 Mar 16; 11 (6): 785. doi: 10. 3390/ plants- 11060785. PMID: 35336667; PMCID: PMC- 8951487.
- Swathi S, Murugananthan G, Ghosh SK. Oviposition deterrent activity from the ethanolic extract of Pongamia pinnata, Coleus forskohlii, and Datura stramonium leaves against Aedes aegypti and Culex quinquefaciatus. Pharmacogn Mag. 2010 Oct; 6 (24): 320- 2. doi: 10. 4103/ 0973- 1296. 71796. PMID: 21120036; PMCID: PMC- 2992147.
References
- Agnivesha, Charaka, Dridhabala. In: Charaka Samhita, ed. Vaidya Jadavaji Trikamji Aacharya, editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2009.
- Sushruta. In: Sushruta Samhita, Sutra Sthana, ed. Vaidya Jadavji Trikamji Acharya, editor. Varanasi: Choukhambha Orientalia; 2005.
- Vagbhata. In: Ashtanga Hrudaya, 9th ed. Anna Moreshwar Kunte, Krishnashastri Navarre, Harishastri, editors. Varanasi: Choukhambha Orientalia; 2005.
- Bhavamishra. In: Bhava Prakasha Nighantu Guduchyadi Varga 11th ed. part 2. Brahma Shankara Mishra, editor. Varanasi: Choukhambha Bharati Academy; 2009.
- Bhavprakasha, commentary by Bulusu Sitaram, forwarded by K.C.Chunekar
- Sharma PV, Kaideva Nighantu. Aushadhi Varga. Chaukhamba Orientalia, Varanasi; 2006.
- Dhanwantri Nighantu, Guduchyadi Varga, Chaukhamba Krishnadas Academy; Varanasi.
- Tripathi I., Raja Nighantu, Prabhadradi Varga, Karveeradi Varga Chaukhamba Krishnadas Academy; Varanasi; 2010
- Shodhala Nighnatu, Haritkyadi varga.
- Priya Nighantu by P. V. Sharma, Haritkyadi Varga Chaukhamba Krishnadas Academy; Varanasi.
- Dr. Gyanendra Pandey, Dravyaguna Vigyana, reprint 2012, Chawkhamba Krishnadas Academy.
- K. Niteshwar Dravyaguna Vigyan, reprint 2017.
- Dr. J.L.N. Sastry and Dr. B.S. Sastry, Dravyaguna Vigyana, Chaukhambha Orientalia, Varanasi.
- Chakrapanidatta, Chakradatta with the Vaidaya Prabha Hindi commentary by Indra Deva Tripathi, Chaukambha Sanskrita Sansthan, Varanasi, 2nd Edition, 1994.
Ayurveda is an Indian system of medicine that is popular since ancient times. Dr. Gupta’s IAFA® has been conducting research studies to find out different phytoconstituents of herbs and their action in the body. Such knowledge acquired by our experts is used in the preparation of medicines and providing the treatment facilities safely and effectively. IAFA® is the provider of safe and effective treatment for a wide range of diseases, mainly allergic diseases all based on Ayurveda.
Was this Page Helpful?
Read More Articles
-

Nimba (Azadirachta indica)
Nimba (Azadirachta indica), known as Neem or Indian Lilac, offers powerful medicinal…
-