Abstract
Background: Seborrheic dermatitis is a chronic inflammatory disorder commonly involving seborrheic areas of the body and presenting with pruritus, erythema, and scaling. In Ayurveda, a closely comparable condition is described as Darunaka, which is categorized under Kapalagata Roga and Kshudra Roga, and attributed mainly to the vitiation of Vata and Kapha Doshas. Classical descriptions highlight manifestations such as Kandu (itching), Rukshata (dryness), Twak-Sphutana (scaling or cracking), and Keshachyuti (hair fall), which align with modern clinical features of seborrheic dermatitis. Seborrheic dermatitis is a chronic, relapsing inflammatory dermatosis of seborrheic areas, comparable to Darunaka described under Kapalagata and Kshudra roga in Ayurveda.
Objective: To evaluate the effect of an integrated Ayurvedic protocol, including external procedures and internal treatment (Chikitsa), in a chronic case of seborrheic dermatitis (Darunaka).
Materials and Methods: A 30-year-old female with a 4-to-5-year history of pruritic and scaly lesions over the scalp and seborrheic body areas was evaluated at IAFA on 18th January 2023. Management included external applications like IAFA E-5 Cell Repair Oil, IAFA Skin Fresh Bar, and IAFA 333 Shampoo, along with internal therapy using Bhoomi Amla and Makoye Swaras, Pitpapra capsules, and IAFA Skin Detox tablets, along with individualized dietary advice. Clinical parameters such as flaking, itching, dryness, and lesion extent were retrospectively graded over four weeks.
Results: Progressive clinical improvement was observed across the four weeks, with a reduction in scalp flaking, i.e., retrospectively graded 3 to 1, itching intensity VAS approximately 8 to 3, and dryness scoring from 3 to 1. No new seborrheic lesions were noted after the third week. The patient also reported improvement in acne activity. Treatment was well tolerated, and no adverse effects were recorded.
Introduction
Seborrheic dermatitis is a common, chronic, relapsing inflammatory skin disease that predominantly affects sebaceous gland–rich areas such as the scalp, face, and various body folds, and typically presents with erythematous, scaly plaques, greasy crusting, and pruritus. Its prevalence in adults is reported between approximately 1–3% in the general population, and higher in specific groups such as individuals with HIV infection or neurological disease.
Dandruff, considered a mild, non-inflammatory form of the same disease spectrum confined to the scalp, affects up to half of the adult population worldwide and shows frequent relapses. Beyond physical discomfort, seborrheic dermatitis can significantly affect quality of life due to visible lesions, chronicity, and psychosocial impact. The pathogenesis of seborrheic dermatitis is multifactorial and not yet fully elucidated.
Current research models highlight an interplay between sebaceous lipid production, overgrowth or qualitative changes of Malassezia spp. on the skin, alterations in the cutaneous microbiome, epidermal barrier dysfunction, and an abnormal or exaggerated host immune response. Malassezia yeasts metabolize sebum lipids and release free fatty acids and other metabolites that can act as irritants and immune triggers, leading to inflammation in susceptible individuals.
Recent work also implicates activation of innate immune pathways, including mast cells, γδ T cells, and the NLRP3 inflammasome, and emphasizes the contribution of skin barrier impairment and microbiome imbalance in disease expression and relapse. Standard management relies mainly on topical antifungals, e.g., azoles, anti-inflammatory agents such as low-potency corticosteroids or calcineurin inhibitors, and medicated shampoos. However, long-term control may be suboptimal, relapses are frequent, and concerns about chronic steroid use remain.
In Ayurveda, conditions closely resembling seborrheic dermatitis and dandruff are described under Darunaka, classified as a Kapalagata Roga, i.e., the disease of the scalp, by Acharya Vagbhata and Sharangadhara, and as a Kshudra roga (minor disease) by Acharya Sushruta, Bhavaprakasha, and Madhava.
Darunaka is attributed primarily to the vitiation of Vata and Kapha doshas and is characterized by Kandu (itching), Rukshata (dryness), Twak-Sphutana (cracking or scaling of the scalp skin), and Keshachyuti (hair fall), features that closely resemble seborrheic scalp disease clinically. Along with this, Ayurvedic literature correlates dandruff and seborrheic dermatitis with Darunaka and highlights the role of faulty diet and lifestyle, excessive use of chemical hair products, and neglect of appropriate oiling and scalp care in precipitating Vata-Kapha aggravation and recurrence.
On this basis, Ayurvedic management of Darunaka generally aims to normalize Vata and Kapha, support Rasa-Rakta-Mamsa Dhatu balance, restore scalp health, and reduce recurrence through a combination of internal formulations, external applications, i.e., medicated oils, shampoos, and pastes, and Pathya-Apathya (dietary and lifestyle) regulation.
Several clinical and conceptual studies have proposed Ayurveda-based treatment protocols for Darunaka with reference to seborrheic dermatitis, but systematically documented case reports with clearly defined outcome parameters remain limited. Documenting individual cases using integrative outcome measures can therefore contribute to the emerging evidence base for Ayurvedic approaches in seborrheic dermatitis and help generate hypotheses for larger controlled studies.
Case Presentation
A 30-year-old female presented with a chronic history of skin rashes and pruritic lesions involving seborrheic regions, including the ears, eyebrows, forehead, neck, breasts, and abdomen, along with persistent scalp flaking and dryness. Symptoms were present for approximately 4-5 years with fluctuating severity and occasional acne formation. The patient reported itching, dryness, and visible scaling that affected cosmetic appearance and caused discomfort during flare-ups.
Clinical evaluation suggested Seborrheic Dermatitis with associated dandruff, which correlated with Darunaka as described in Ayurveda due to Vata-Kapha predominance. No significant medical comorbidities were mentioned at the time of the consultation. Ayurvedic therapy was initiated at IAFA, and progressive clinical improvement was observed over the following weeks.
1) Patient Details
Age/Sex: 30-year-old / Female
Date of first visit: 18th January 2023
2) Chief Complaints
- Skin rashes with itching
- Dryness involving the ears, eyebrows, forehead, neck, breasts, and abdomen
- Scalp flakes with itching
- Acne
3) Diagnosis
Modern Diagnosis: Seborrheic Dermatitis with dandruff
Ayurvedic Diagnosis: Darunaka -Kapalagata or Kshudra Roga, i.e., Vata-Kapha Pradhana
4) Triggers and Exacerbating Factors
- Dryness of the skin and scalp aggravated itching and flaking
- Cold and dry seasons are associated with the worsening of seborrheic symptoms
- Possible Kapha-aggravating dietary factors and lifestyle patterns
- Cosmetics and hair products may irritate the scalp and worsen scaling
- Stress and seasonal variations may contribute to flare-ups
Materials and Methods
1) Intervention Protocol
Ayurvedic treatment was initiated after consultation on 18th January 2023 at IAFA, with a focus on the management of Vata-Kapha vitiation, normalization of scalp integrity, Kleda Shoshana, Rakta-Mamsa support, and reduction of inflammatory and scaling tendencies. Treatment included external applications and internal treatment, along with dietary modifications intended to minimize Kapha aggravation and dryness of the skin and scalp.
2) Ayurvedic Diagnostic Framework
Table 1. Ayurvedic Diagnostic Analysis (Samprapti Ghataka)
| Samprapti Ghataka | Analysis |
| Dosha | Vata- Kapha Pradhana |
| Dushya | Rasa and Rakta predominance, with Mansa involvement at the scalp and skin |
| Strotas | Rasavaha and Raktavaha Strotas, Twaka-gata involvement |
| Strotodushti | Sanga (scaling and obstruction), Rukshata, and mild local inflammation |
| Udbhava Sthana | Kapalagata (scalp region) |
| Vyaktasthana | Scalp, eyebrows, ears, face, upper trunk, and abdominal region |
| Roga Marga | Bahya Roga Marga (skin and scalp) |
| Adhishthana | Twak (skin) and Kapala (scalp) |
3) Ayurvedic Treatment Protocol
The therapeutic plan focused on reducing Vata-Kapha derangement in the body, improving scalp barrier, mitigating inflammatory response, and modulating microbial imbalance. External therapy consisted of IAFA E-5 Cell Repair Oil, IAFA Skin Fresh Bar, and IAFA 333 Shampoo, intended for skin repair, anti-inflammatory action, anti-scaling support, and reduction of itching.
Internal therapy included Bhoomi Amla Swaras, Makoye Swaras, Pitpapra capsules, and IAFA Skin Detox tablets, supporting detoxification, anti-allergic action, blood purification, and reduction of itching and dryness. Together, these internal and external treatments are aimed at restoring scalp health, reducing recurrence, normalizing dryness, preventing cracking, and improving overall dermatological comfort without adverse effects.
4) Treatment Progression and Formulations
Table 2. Formulations Used with Dose, Frequency, Route, and Duration
| Formulation | Dose | Frequency | Route | Duration |
| IAFA E-5 Cell Repair Oil | The 10 ml formulation is mixed in 10 ml of extra virgin coconut oil | Once or twice daily | Topical | Continuous |
| IAFA Skin Fresh Bar | As directed | Once daily | Topical | Continuous |
| IAFA 333 Shampoo | As directed | Once daily or as needed | Topical | Continuous |
| Bhoomi Amla Swaras | 30 ml of water | Twice daily | Oral | Continuous |
| Makoye Swaras | 30 ml of water | Twice daily | Oral | Continuous |
| Pitpapra Capsule | 1 capsule | Twice daily | Oral | Continuous |
| IAFA Skin Detox Tablet | 2 tablets | Twice daily | Oral | Continuous |
5) Phased Therapeutic Strategy
The treatment was given in phases according to symptom response and tissue healing requirements. Initial care emphasized controlling itching, scaling, and dryness. Subsequent weeks focused on stabilizing the inflammatory response, reducing lesion spread, improving barrier function, and preventing recurrence.
Table 3. Phased Ayurvedic Treatment Strategy
| Phase | Timeline | Ayurvedic Treatment | Objective | Patient Response |
| Phase 1: Initial Management | Week 1 | External and internal treatment | Reduce itching, scaling, and dryness | Visible reduction in flakes and pruritus |
| Phase 2: Stabilization | Week 2-3 | Continued external and internal treatment | Preventing new lesions and controlling inflammation | No new seborrheic lesions after week 3 |
| Phase 3: Maintenance | Week 4 | Same protocol and diet regulation | Maintain barrier function, reduce recurrence | Progressive improvement and tolerance |
6) Monitoring and Evaluation Protocol
Evaluation was based on clinical symptoms, scalp involvement, and retrospective grading of response parameters, including itching (VAS), flaking severity (0–3), dryness (0–3), and lesion extent. Overall tolerability and absence of adverse effects were monitored during contact follow-up.
Table 4. Clinical response
| Parameter | Baseline | Week 2 | Week 4 |
| Flaking (0–3) | 3 | 2 | 1 |
| Itching VAS | 8 | 5 | 3 |
| Dryness (0–3) | 3 | 2 | 1 |
| New lesions | present | occasional | none |
Table 5. Clinical Monitoring Approach
| Parameter | Assessment Method |
| Scalp flaking (0–3) | Retrospective grading |
| Itching VAS (0–10) | Retrospective VAS |
| Dryness (0–3) | Retrospective grading |
| New lesion appearance | Clinical observation |
| Tolerability | Patient feedback |
7) Dietary and Lifestyle Measures
- Light and easily digestible diet
- Bitter and astringent foods
- Lukewarm water at intervals
- Fruits, millets, and green vegetables
- Avoidance of A1 milk, gluten-rich items, fried foods, excess spice, sour foods, fermented items, and seafood
Results
At baseline, the patient presented chronic seborrheic dermatitis involving the scalp and multiple seborrheic regions, characterized by flaking i.e., grade 3, itching in VAS- approximately. 8/10, and dryness of grade 3. Following initiation of the Ayurvedic treatment protocol at IAFA, a progressive improvement was documented across all clinical parameters during the four-week observation period.
Symptomatic reduction was most notable in scalp scaling and itching within the first two weeks, followed by stabilization and absence of new lesions in the subsequent period. By week three, progression of existing lesions ceased, and cosmetic improvement, along with reduction in pruritus, was reported. By week four, flaking reduced to grade 1, itching to approximately 3/10, and dryness to grade 1. Acne activity, initially present along with seborrheic features, also reduced by the end of treatment. No adverse effects or treatment-related intolerance were reported.
Clinical progress was supported further by patient-reported comfort in scalp integrity, decreased visible flakes during hair washing, and improved appearance of previously affected areas such as ears, eyebrows, and forehead. The patient also reported greater social confidence due to better control of scalp scaling.
Graphical Representation
Figure 1. Reduction in Scalp Flaking Severity Over 4 Weeks

Line graph showing progressive decline in flaking score from 3 at baseline to 1 at week 4, demonstrating marked symptomatic improvement and stabilization after week 2. The Y-axis shows Flaking score (0–3), and the X-axis shows Baseline, Week 2, and Week 4.
Figure 2. Itching Severity (VAS) Over 4 Weeks

Patient-reported VAS scores demonstrated a steady reduction from 8/10 at baseline to 3/10 at week 4, indicating symptomatic relief. Y-axis showing VAS score and X-axis showing Time (weeks).
Figure 3. Skin Dryness Scores Over Time
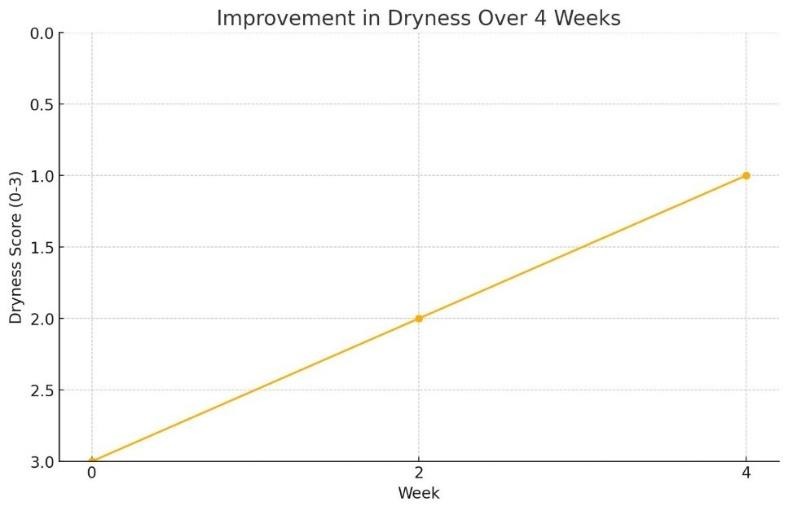
Dryness scores improved from grade 3 at baseline to grade 1 by week 4, reflecting improved scalp barrier and moisturization associated with external therapy. Y-axis showing Dryness (0–3) and X-axis showing Time (weeks).
Figure 4. Appearance of New Lesions (Presence vs Absence)

Bar graph illustrating reduction from present at baseline to none by week 4, indicating control and suppression of exacerbations.
The Ayurvedic treatment demonstrated clinical benefit across various parameters, including flaking, itching, dryness, and lesion propagation, with marked symptomatic relief achieved by week 4 and no adverse outcomes. Absence of new lesions from week three onwards signifies disease stabilization, while concurrent improvement in acne activity suggests systemic modulation rather than purely topical effect. These results indicate the potential therapeutic utility of Ayurvedic external and internal treatment in chronic seborrheic dermatitis (Darunaka).
Discussion
Seborrheic dermatitis is an inflammatory dermatological condition with an etiology involving Malassezia overgrowth, altered skin lipid metabolism, epidermal barrier dysfunction, and immune-mediated inflammation. As per Ayurveda, it can be correlated to Darunaka, primarily characterized by Vata-Kapha vitiation with symptoms such as Kandu (itching), Rukshata (dryness), Twak-Sphutana (scaling), and Keshachyuti.
The chronicity and recurrence observed in modern dermatology parallel the classical descriptions of repeated scalp irritation due to disturbed Kapha and dryness of Vata. The therapeutic objective in this case, therefore, emphasized Dosha Samyata, Kleda Shoshana, Rakta-Mamsa support, removal of subtle Aama (toxins), and restoration of scalp barrier integrity. The treatment strategy applied combined external and internal Ayurveda-based formulations in alignment with Samprapti Vighatana, i.e., breaking pathogenesis.
External agents, including IAFA E-5 Cell Repair Oil, IAFA Skin Fresh Bar, and IAFA 333 Shampoo, collectively aimed to reduce inflammation, improve epidermal barrier, normalize scalp moisture, and decrease microbial load. Internal medications such as Bhoomi Amla Swaras, Makoye Swaras, Pitpapra capsules, and IAFA Skin Detox tablets were selected due to their known anti-allergic, anti-inflammatory, and blood-purifying properties, with an objective of detoxification and Rakta-Mamsa Dhatu support.
1) Ayurvedic Pathophysiological Understanding
In Darunaka, the fundamental pathology arises from Vata-Kapha vitiation within the Kapala and Twak, where Vata creates excessive dryness, roughness, and scalp cracking, while Kapha leads to coating, inflammation, itching, and recurrent flaking. The presence of Ama (toxins) further obstructs the microchannels, weakens local immunity, and sustains chronic episodes of irritation.
The formulations used in this case directly counter this Samprapti through coordinated actions, i.e., external applications rich in Pongamia, Berberis, Wrightia, Psoralea, Cassia fistula, and coconut-based emollients, etc., soothe inflammation, reduce Kapha-derived scaling, and restore Snigdha Guna to correct Vata-induced dryness, thereby repairing the scalp barrier.
Internal therapy with Bhoomi Amla, Makoye, and Pitpapra Swaras provides Raktashodhaka and Daha-shamana effects, reducing irritative heat and pruritus, while Pitpapra offers classical Kusthaghna action to calm chronic skin reactivity.
The Skin Detox Tablet, containing Khadira, Tinospora, Triphala, and Karanja, promotes Aama-Pachana, Kapha-Vata Shamana, and Twak- Strotoshodhana, improving tissue metabolism and preventing further obstruction. Together, these formulations balance the Doshas, cleanse inflammatory metabolites, nourish the scalp tissues, and restore normal Twak physiology, effectively breaking the pathogenesis of Darunaka and supporting sustained symptom resolution.
Table 6: Formulations, Key Ingredients, and Their Actions
| Formulation | Key Ingredients | Ayurvedic Actions | Modern Pharmacology |
| IAFA E-5 Cell Repair Oil | Pongamia glabra, Albizia lebbeck, Berberis aristata, Cassia fistula, Cocos nucifera | Kandughna, Vranaropana, Keshya, etc. | Antifungal, anti-inflammatory, antioxidant, barrier-repair emollient |
| IAFA Skin Fresh Bar | Sveta Kutaj, Neelini, Kumari, Lodhar, Nimba, Chakramarda, Almond oil, Avocado oil, Coconut oil | Twachya, Krimighna, Shothahara, Raktaprasadana | Antimicrobial, anti-allergic, antioxidant, moisturizing lipid support |
| IAFA 333 Shampoo | Aloe barbadenis, Acacia concinna, Trigonella foenum, Hibiscus rosasinensis, Wrightia tinctoria, Psoralea corylifolia, Triphala, Cassia fistula, Pongamia glabra, Cassia tora, Indigofera tinctoria, Berberis aristata | Kandughna, Keshya, Kapha-Vata Shamaka, Tvak-Shodhaka | Antifungal, keratolytic, anti-inflammatory, scalp microbiome modulation |
| Bhoomi Amla Swaras | Phyllanthus niruri | Raktashodhaka, Dahashamaka, Kandughna | Anti-inflammatory, hepatoprotective, antipruritic |
| Makoye Swaras | Solanum nigrum | Dahashamana, Shothahara, Kandughna | Anti-inflammatory, antipruritic, soothing effect |
| Pitpapra Capsule | Fumaria indica | Kusthaghna, Daha-Shamana, Trishnahara | Antioxidant, anti-inflammatory, and skin disease supportive |
| IAFA Skin Detox Tablet | Adathoda vasica, Melia azedarach, Solanum surattense, Trichosanthes dioica, Tinospora cordifolia, Pongamia glabra, Triphala, Mahamanjistadi Kwath | Rakta-Shodhana, Krimighna, Kandughna, Ama Pachana, Dosha-Shamana | Anti-inflammatory, antimicrobial, immunomodulatory, detoxifying |
Happy Note
Source:- https://g.co/kgs/UQxwCG
Conclusion
This case showed that using a combination of Ayurvedic internal medicines and external applications helped reduce itching, flaking, dryness, and new lesion formation in a patient with chronic seborrheic dermatitis (Darunaka). The treatment was well-tolerated, and no side effects were reported.

The improvement suggests that Ayurvedic management aimed at balancing Vata and Kapha, supporting the skin barrier, and reducing inflammation may be useful in similar cases. However, this is a single case, and more studies with longer follow-up and larger numbers of patients are needed to confirm how effective this approach is in the long term.
References
- Dall’Oglio, Federica & Nasca, Maria & Gerbino, Carlo & Micali, Giuseppe. (2022). An Overview of the Diagnosis and Management of Seborrheic Dermatitis. Clinical, Cosmetic and Investigational Dermatology. 15. 1537- 1548. 10. 2147/ CCID. S284671.
- Navarro Trivino FJ, Velasco Amador JP, Rivera Ruiz I. Seborrheic Dermatitis Revisited: Pathophysiology, Diagnosis, and Emerging Therapies-A Narrative Review. Biomedicines. 2025 Oct 9; 13 (10): 2458. doi: 10. 3390/ biomedicines 13102458. PMID: 41153741; PMCID: PMC- 12562114.
- Goyal, Swati & Verma, Nitin. (2024). A Conceptual Recapture of Darunaka and Its Relevance in the Present Era. International Journal of Ayurveda and Pharma Research. 126- 131. 10. 47070/ ijapr. v12i7. 3332.
- Madan, Poonam & Rathi, Bharat & Dhote, Sachin & Wairagade, Sonali & Swati, S & Gadgil, Swati & Sameer, Manohar & Joshi, (2021). An Ayurvedic Approach in the Management of Darunak (Dandruff) -A Review. 8. 1315- 1320.
- Kadegaon, Mohasin. (2023). The Ayurvedic Management of Darunaka with Special Reference to Seborrheic Dermatitis -A Single Case Report. Vol 8. 556- 559. 10. 1729/ journal. 32837.
- Dall’Oglio F, Nasca MR, Gerbino C, Micali G. An Overview of the Diagnosis and Management of Seborrheic Dermatitis. Clin Cosmet Investig Dermatol. 2022 Aug 6; 15: 1537- 1548. doi: 10. 2147/ CCID. S284671. PMID: 3596- 7915; PMCID: PMC- 9365318.
- Borda LJ, Perper M, Keri JE. Treatment of seborrheic dermatitis: a comprehensive review. J Dermatolog Treat. 2019 Mar; 30 (2): 158- 169. doi: 10. 1080/ 09546634. 2018. 1473554. Epub 2018 May 24. PMID: 2973- 7895.
- Vidal SI, Menta N, Green L. Child and Adult Seborrheic Dermatitis: A Narrative Review of the Current Treatment Landscape. Dermatol Ther (Heidelb). 2025 Mar; 15 (3): 599- 613. doi: 10. 1007/ s13555- 025- 01351- z. Epub 2025 Feb 14. PMID: 3995- 3371; PMCID: PMC- 11909311.
- Vijay, Krishnan, & Sumit, Nathani, Rabadiya. (2025). AN AYURVEDIC APPROACH TO MANAGING DARUNAKA: INSIGHTS FROM A CASE STUDY. International Ayurvedic Medical Journal. 13. 1494- 1500. 10. 46607/ iamj- 3513- 052025.
- Jain, Pranjal & Nakil, Amey & Chandurkar, Vivek. (2021). A UNIQUE COMBINATION OF AYURVEDIC MEDICINES AND PANCHAKARMA IN THE MANAGEMENT OF DARUNAKA: A SINGLE CASE STUDY. AYUSHDHARA. 3225- 3228. 10. 47070/ ayushdhara. v8i2. 724.
- Galizia, G., Belloni Fortina, A., & Semenzato, A. (2024). Seborrheic Dermatitis: From Microbiome and Skin Barrier Involvement to Emerging Approaches in Dermocosmetic Treatment. Cosmetics, 11 (6), 208. https:// doi. org/ 10. 3390/ cosmetics/ 11060208
- Borda LJ, Wikramanayake TC. Seborrheic Dermatitis and Dandruff: A Comprehensive Review. J Clin Investig Dermatol. 2015 Dec; 3 (2): 10. 13188/ 2373- 1044. 1000019. doi: 10. 13188/ 2373- 1044. 1000019. Epub 2015 Dec 15. PMID: 27148560; PMCID: PMC- 4852869.
- Araya M, Kulthanan K, Jiamton S. Clinical Characteristics and Quality of Life of Seborrheic Dermatitis Patients in a Tropical Country. Indian J Dermatol. 2015 Sep- Oct; 60 (5): 519. doi: 10. 4103/ 0019-5154. 164410. PMID: 2653- 8714; PMCID: PMC- 4601435.
- Gary G. Optimizing treatment approaches to seborrheic dermatitis. J Clin Aesthet Dermatol. 2013 Feb; 6 (2): 44- 9. PMID: 2344- 1240; PMCID: PMC- 3579488.
- Asz-Sigall, Daniel & Tosti, Antonella. (2020). Seborrheic Dermatitis. 10. 1007/ 978- 3-030- 21555- 2- 12.








