On This Page
Summarise this article using AI
Introduction
In the normal collection of the intestinal microorganism, fungi are the essential part although they contribute 0.1% to 1% of all fecal microbes. Among fungi, candida species colonization rate ranges from 30- 70% among healthy adults which makes them normal inhabitants of the gastrointestinal (GI) tract. It is also true that genus Candida is the most altered fungal composition in intestinal diseases.
Are you suffering from indigestion, abdominal pain, diarrhea, persistent bloating, fatigue, or recurrent intestinal fungal infections? You might be dealing with intestinal candidiasis, a condition caused by the overgrowth of Candida fungi in the digestive tract, which disrupts the gut flora and results in various digestive and systemic symptoms.
In Ayurveda, Intestinal candidiasis can be correlated with Krimi Roga which occurs due to an imbalance of Dosha specifically Pitta and Kapha Doshas which results in weak digestive fire (Manda Agni), excessive fermentation in the digestive system, toxins (Ama) accumulation, which creates a favorable environment for fungal overgrowth in the intestine.
Ayurvedic Treatment for Intestinal Candidiasis focuses on restoring digestive system balance through the use of digestive stimulants i.e. Deepana and Pachana Dravya, Anti-fungal herbs (Krimighana Dravya), use of various detoxification therapies (Panchakarma), and personalized Pitta-Kapha pacifying diet, Yoga therapy, etc.
If you are suffering from the above-mentioned diseases, don’t worry, Dr. Sahil Gupta at IAFA Ayurveda can help you with an Ayurvedic approach to eliminate candida fungi naturally and restore digestive system health.
Understanding of Human Gut Mycobiome
Approximately 40 trillion cells inhabit the human intestinal tract, making it the best home for microorganisms. In this ecosystem of microorganisms, bacteria form the major part and the fungal community is smaller in proportion, but it plays an important role in maintaining gut health and also contributes to disease when imbalanced in the intestine.
As per the recent genomic analysis, fungi constitute only approximately 0.1-1% of the total gut microbiota, but due to their larger cell size and metabolic activity, they play a major role in physiological and pathological processes. The adult gut mycobiome is predominantly composed of various Candida species, mainly Candida albicans, followed by Saccharomyces cerevisiae, Candida tropicalis, Candida parapsilosis, Candida glabrata, etc.
Most studies revealed that various fungal compositions are present in individuals with the disease, but even in healthy individuals, Candida species remain dominant, indicating their natural presence in the human digestive system.
Understanding this fungal ecosystem is essential to identifying imbalances like intestinal candidiasis and treating them deep from the roots in Ayurveda, which views microbial imbalances through the dosha disturbance and toxin (Ama) accumulation in the body.
What is Intestinal Candidiasis?
The over-fungal growth condition is primarily caused by Candida species, which normally live in the gastrointestinal tract in small amounts. Under normal situations, the gut microbiome maintains a balance between fungi and bacteria residing inside the digestive system.
However, when the imbalance is created due to various factors like prolonged use of antibiotics, immunosuppression, chronic illness, excessive intake of high-sugar diets, stress, etc. The Candida species increase excessively in the gut. This overgrowth may result in various symptoms of systemic inflammation, compromised immunity, etc.
What is Intestinal Candidiasis – As Per Ayurveda?
In Ayurveda, intestinal candidiasis can be correlated to disease caused by pathogenic organisms (Krimi Roga) and toxins (Ama) due to undigested food accumulation (Apakva Aahar) in the gastrointestinal tract.
Along with this, it is associated with an imbalance of Pitta and Kapha doshas, where imbalanced digestive fire (Mnadagni) leads to fermentation in the digestive tract which creates an environment best for microbial overgrowth.
What is Small Intestinal Fungal Overgrowth (SIFO)?
A gastrointestinal condition in which excessive growth of fungi occurs in small intestines is known as Small Intestinal Fungal Overgrowth (SIFO). The fungi that are involved in it are mainly candida species and this results in abdominal discomfort, irregular bowel movements, constipation, etc. Weakened immunity, excessive use of proton pump inhibitors, etc. increased the chances of SIFO in the individual.
Are Small Intestinal Fungal Overgrowth (SIFO) and Intestinal Candidiasis the Same Diseases?
No, SIFO and Intestinal Candidiasis are not the same, but they are related to each other. The key differences between SIFO and Intestinal Candidiasis are as follows:-
- When fungal overgrowth occurs, especially candida in the small intestine, then it is known as SIFO, whereas when candida grows in any part of the intestine (i.e., can affect the small intestine and large intestine) both then it is known as Intestinal Candidiasis.
- Intestinal candidiasis is a broad condition including SIFO as part of it. Along with this, SIFO has symptoms like bloating, abdominal discomfort, diarrhea, etc,. whereas intestinal candidiasis has SIFO symptoms along with fatigue, sugar craving, brain fog, etc.
Who Gets Affected by Intestinal Candidiasis?
Any factor that disturbs the natural balance of the gut flora or the factors that weaken the immune system cause Intestinal Candidiasis. Intestinal Candidiasis can affect anyone, but the factors mentioned below are more prone to Intestinal Candidiasis:-
- Frequent and overuse of antibiotics as they kill both bad and good bacteria and give candida a chance to grow.
- Individuals with weak immune systems due to overuse of steroids, immunosuppressive drugs, etc.
- The patient is undergoing chemotherapy.
- Diabetic people are more prone to Intestinal Candidiasis, as high blood sugar promotes fungal growth.
- Individuals with leaky gut syndrome are more affected by intestinal Candidiasis.
- Infants who are fed formula milk early or those who are born by C-section are also affected by these diseases.
- A stress-prone person is more affected by Intestinal Candidiasis.
- Individuals who overuse antacids like proton pump inhibitors frequently.
How Common is Intestinal Candidiasis?
The prevalence of Intestinal Candidiasis is more common in populations with poor nutrition. The exact prevalence of Intestinal Candidiasis is not precise and data is also scarce, but a survey study revealed a significant burden of intestinal Candidiasis in ICU patients that is approximately 4- 5 % and in hospitalized neonates approximately 2%.
Types of Intestinal Candidiasis
- Superficial Candidiasis: Superficial candidiasis affects the mucosal lining of the intestine and is considered the mild form of intestinal candidiasis. It is more commonly found in people after the use of antibiotics and in individuals who are suffering from dysbiosis. It includes symptoms like abdominal discomfort, bloating, gas, etc.
- Invasive Candidiasis: When the candida infection affects deeper tissues and may enter the bloodstream known as candidemia, it is known as invasive candidiasis. It is life-threatening and is mainly seen in immunocompromised patients like HIV patients, cancer patients, etc.
- Chronic Intestinal Candidiasis: Chronic intestinal candidiasis often overlaps with systemic candidiasis and occurs due to long-term antibiotics use, weak immunity, high sugar diets, etc. Its symptoms include sugar cravings, digestive discomfort, brain fog, etc.
- Iatrogenic Candidiasis: This type of intestinal candidiasis is common in post-operative and hospitalized patients and is caused by overuse of antibiotics, chemotherapy, and use of corticosteroids.
- Candida Colitis: Candida Colitis mimics IBD-like symptoms i.e. mucus in stool, abdominal pain, diarrhea, etc. and it mainly affects the colon part of the large intestine. For diagnosis of candida colitis biopsy and colonoscopy are done.
- Small Intestinal Fungal Overgrowth (SIFO): It is also known as Focal Candida Overgrowth which is localized fungal overgrowth commonly seen in the small intestine and its symptoms include nausea, altered bowel habits, nausea, etc.
Causes of Intestinal Candidiasis (Modern Aspect)
- Frequent use of antibiotics
- Prolonged use of antibiotics
- Uncontrolled high blood sugar level
- Intake of a diet rich in simple carbohydrates
- Immune suppression is due to diseases like cancer, AIDS, etc.
- Overuse of corticosteroids
- Oral contraceptives sue
- Hormonal imbalance in early pregnancy
- Stress
- Poor lifestyle
- Suffering from diseases like Ulcerative colitis, Crohn’s disease, etc.
Causes of Intestinal Candidiasis – As Per Ayurveda
- Weak digestive fire (Manda Agni) due to intake of heavy food (Guru Bhojana), excessive intake of sweet and oil foods (Ati Madhur and Snigdha Aahara), eating before the previous meal is digested (Adhyashana), excessive intake of water (Atyaambupana), etc.
- Improper eating habits (Vishmashana) lead to improper digestion, which results in the accumulation of toxic substances (Ama) and makes the gut fertile ground for pathogenic organisms like candida.
- Excessive consumption of curd (Dadhi), sweets (Madhura), fermented foods, or improperly cooked food (Ardha Pakva Aahara).
- Day sleeping (Diwa Swapana)
- Weaknesses of the metabolic fire of tissues, i.e., Dhatu Agni Mandya, mainly of Rasa and Rakta dhatu, due to overeating, eating during indigestion (Ajirna), or intake of Mithya Aahara (improper diet), etc.
- Suppression of natural urges (Vega Dharana)
- Improper contact of senses with object, i.e. Asatmya Indiryartha Sanyoga, etc.
- Shukra dushti or Artava dushti: If candidiasis affects the genital tract, then it may involve the gut some time or vice versa.
- Parasitic infestation (Krimi) due to an imbalance in gut flora.
Symptoms of Intestinal Candidiasis (Modern Aspect)
- Bloating
- Gas
- Abdominal pain or cramps
- Diarrhea
- Constipation
- White coated tongue
- Indigestion
- Foul smell of stool
- Sugar cravings
- Mood swings
- Depression
- Fatigue
- Lethargy
- Skin issues like itching, rashes, eczema, etc.
- Sometimes females may have recurrent urinary infections and vaginal infections.
Symptoms of Intestinal Candidiasis – As Per Ayurveda
- Feeling cold (Shaitya)
- Heaviness in the body (Gourvata)
- Constipation (Mala Sanga)
- Loose stools (Ati Mala Pravriti)
- Sweet breath or foul breath (Mukha Madhrya ya Mukha Madhurta)
- Abdominal pain (Udar Shula)
- Bloating (Aadhmana)
- Drowsiness (tundra)
- Mild respiratory symptoms sometimes coexist like Shwasa and Kasa
- Mental fatigue, mood disturbances (Mano Dourbalaya)
- Loss of appetite (Aruchi)
- Indigestion (Ajeerna)
- Itching around the anal region (Guda Kandu)
- Excessive sleepiness (Ati Nidra)
- Laziness (Aalasya)
- Weaknesses (Dourbalya)
- Weak digestion (Mandaagni)
- Fever (Jwara)
Diagnosis of Intestinal Candidiasis – As Per Ayurveda
As per Ayurveda the diagnosis of intestinal candidiasis is made by diseases and patient examination i.e. Roga and Rogi Pariksha and for this three-fold examination (Trividha Pariksha) is done by inspection (Darshana) (observing the white coated tongue, bloating, etc.), palpation (Sparshana) (pulse examination, abdominal tenderness, etc.), interrogation (Prashana) about symptoms, use of antibiotics and diet and lifestyle history, along with this eightfold examination is also done (vary from person to person) to make a diagnosis. Diagnosis is further supported and confirmed by laboratory examinations like stool test, blood test, urine organic acid test, and in severe cases with biopsy and endoscopy, etc.

“Dr. Gupta’s IAFA is the best Ayurveda centre for the treating Intestinal candidiasis through natural friendly Ayurvedic measures”.
Reach Institute of Applied Food Allergy® for a natural friendly and Ayurvedic skin rejuvenation!!!
– Dr. Sahil Gupta (B.A.M.S., M.H.A.)
Ayurvedic Allergy Specialist
CEO & Founder of IAFA®
At last, Easier Intestinal Candidiasis Management
Trusted by
More than 90,000 Patients
Convenient
at-Home Treatments
9.2 / 10
Customer Satisfaction Score
Intestinal Candidiasis Ayurvedic Treatment
Dr. Sahil Gupta at IAFA Ayurveda offers Intestinal Candidiasis Ayurvedic treatment by detoxification therapy, the use of various herbs and formulations, personalized dietary and lifestyle modifications, Yoga therapy and gem therapy, etc.
Ayurvedic treatment for Intestinal Candidiasis provided by IAFA Ayurveda helps in eliminating the root cause of intestinal candidiasis i.e. toxin (Ama), the weak digestive fire (Agnimandya), pathogens (Krimi) and helps in restoring balance to your gastrointestinal system.
Detoxification Therapy (Shodhana Therapy) for Intestinal Candidiasis
For detoxification of the individual suffering from intestinal candidiasis first appetizers and digestive stimulants are used i.e. Deepana and Pachana Dravya like Trikatu, and Chitrakadi Vati which possess antifungal activities, prokinetic actions, etc. Which helps in reducing candida infection and also helps in improving weak digestive fire and digestion.
- Purgation therapy (Virechana) – Therapeutic purgation is done in intestinal candidiasis patients with the help of various herbs to cleanse the intestine and eliminate Kapha and Pitta Dosha. By using various formulations like Gandharvahastadi Kashaya, Avipattikar Churna, Eranda Taila (castor oil), colon cleansing along with acidity balance, etc. is done by proven anti-candida effects of active ingredients like ricinoleic acid which does not only reduce fungal growth but also regulate intestinal peristalsis.
- Medicated Enema Therapy (Basti) – In this process, medicated oil or decoctions are administered through the rectum and are useful in symptoms like constipation, abdominal discomfort, bloating, etc. by the drugs and formulations that are used in it like Dashmoola Taila, Triphala decoction, etc. which possess anti-inflammatory, immunomodulatory effect for restoring balance in the gut flora.
Herbs for Intestinal Candidiasis
Herbs for Intestinal Candidiasis Ayurvedic treatment includes like Triphala – combination of three fruits – Haritaki (Terminalia chebula), Bibhitaki (Terminalia bellerica), Aamlaki (Emblica officinalis), Neem (Azadirachta indica), Vidanga (Embelia ribes), Guduchi (Tinospora cordifolia), Garlic (Allium sativum), Mustaka (Cyperus rotundus), Haridra (Curcuma longa), Kutaja (Holarrhena antidysenterica), etc.
These herbs possess antioxidant, anti-fungal, anti-microbial, anti-inflammatory, immunomodulatory, anti-candida, gut protective activities, etc., which inhibit Candida albicans biofilm formation and support healthy and balanced gut flora.
They also help to treat intestinal candidiasis by disrupting fungal cell walls, inhibiting the growth of Candida albicans filamentation, supporting gut mucosal healing, etc. These herbs are considered as the top herbs that can be used in the treatment of the intestinal candidiasis.
Gem Therapy for Intestinal Candidiasis
Few stones are recommended to wear in intestinal candidiasis, as per Vedic Astrology. These stones can be worn after proper consultation with an astrologer as per your birth date, Zodiac sign, etc, to get only benefits.
As per astrology, Emerald (Panna), Red Coral (Moonga), Pearl (Moti), and Yellow Sapphire (Pukhraj) can be worn as per your natal chart if you are suffering from Intestinal candidiasis.
These stones help in balancing Vata and Kapha, boost metabolism and immunity, enhance blood circulation, reduce stress-induced gut symptoms, enhance gut-brain axis healing, and help in fighting fungal overgrowth.
Committed to Holistic Healing through Alternative Medicine Since 2008
Diet and Lifestyle Guidance (Pathya-Apathya) for Intestinal Candidiasis
According to Ayurveda, if your diet is correct, then medicine is of no use because a good gut is considered the basis of a healthy individual. So, by giving attention to our daily diet, we not only get relief from the diseases from which we suffer but also avoid the upcoming diseases. Below, we mention some dietary and lifestyle guidelines that one can follow for intestinal candidiasis:-
What to Do (Pathya) in Intestinal Candidiasis?
- Light food that is easy to digest should be taken (Laghu Aahara)
- Bitter vegetables (Tikta Shaka) and astringent (Kashaya) food should be included in the diet, like Patola, Triphala, etc.
- Use digestive herbs in the diet like Ajwain, Jeera, Hinga, dry ginger, etc.
- Old cereal and grains (Purana Dhanya) should be taken into the diet
- Medicated buttermilk should be included in the diet.
- Warm water and herbal decoction should be included in the diet.
- Anti-fungal foods like garlic, turmeric, ginger, oregano, clove, etc. should be included in the diet.
- High-fiber food should be eaten like flax seeds, green leafy vegetables, etc.
- Lean protein should be added to the diet, like legumes, Moong Dal, etc.
- Yoga, meditation, and exercise should be done regularly.
- Regular bowel habits should be maintained.
What to Avoid (Apathya) in Intestinal Candidiasis?
- Avoid heavy meals (Guru Bhojana)
- Avoid incompatible food (Virrudha Aahara)
- Avoid Abhishyandi Aahara like curd, cheese, milk at night, etc.
- Alcohol and smoking should be avoided.
- Fermented food should be avoided like Idli, dosa, etc.
- Processed food and junk food should be avoided.
- Anger and anxiety (Krodha and Shoka) should be avoided.
- Daytime sleeping (Diwa Swapana), and night awakening (Ratri Jagarana) should be avoided.
- Sugar, honey, and jaggery should be avoided.
- A sedentary lifestyle should be avoided.
Yoga Asanas for Intestinal Candidiasis
Various Yoga Asanas like Wind relieving pose (Pawanmuktasana), Half spinal twist pose (Ardha Matsyendrasana), Bow pose (Dhanurasana), Diamond pose (Vajrasana), Seated forward bend (Paschimottanasana), Triangle pose (Trikonasana), Bridge pose (Setu Bandhasana), Cat cow pose (Marjari Asana – Bitilasana), Skull shining breath (Kapalbhati), Deep breathing technique (Pranayama) like Bhramari parnaayama, Meditation, etc. can be done in intestinal candidiasis.
These Yogic Asanas stimulate abdominal organs, prevent toxin formation (Ama), relieve constipation, improve gut motility, relieve gas, support detoxification, enhance oxygen supply to the gut, activate the Vagus nerve which enhances gut healing, regulate the HPA axis (hypothalamic pituitary adrenal axis) which helps in decreasing fungal overgrowth.

Frequently Asked Questions
Question) Does Ashwagandha Fight Candida?
Answer) Ashwagandha is not a direct anti-fungal herb, but it can help indirectly by boosting immunity, reducing stress, and supporting the gut balance of the individual.
Question) How to Treat Gut Candida Naturally and Permanently?
Answer) By detoxification therapy, following an anti-candida diet, and using natural antifungals. By reducing stress and avoiding the main culprit overuse and frequent use of antibiotics one can treat candida naturally and permanently.
Question) What Vitamin Deficiency Causes Candida Overgrowth?
Answer) Deficiency of Vitamin D, B6, B12, iron, and zinc can weaken immunity, which as a result makes the body more prone to Candida overgrowth.
Question) Is Candida Overgrowth Contagious?
Answer) It develops due to internal imbalance, especially in the gut flora of the body, not by contact with infected individuals.
Question) Can Candida Overgrowth Return?
Answer) Yes, if underlying causes of improper diet, stress, and frequent overuse of antibiotics are not treated deep from the roots, then its recurrence can occur.
References
- Oyom AP, Okello E, Acam V, Aramo C, Mwambi B, Okiria JC, Oyet C. Prevalence and antifungal susceptibility of gastrointestinal candidiasis among diabetic patients: A cross-sectional study. Afr J Lab Med. 2020 Dec 10; 9 (1): 997. doi: 10. 4102/ ajlm. v9i1. 997. PMID: 3335- 4526; PMCID: PMC- 7736660.
- Kreulen IAM, de Jonge WJ, van den Wijngaard RM, van Thiel IAM. Candida spp. in Human Intestinal Health and Disease: More than a Gut Feeling. Mycopathologia. 2023 Dec; 188 (6): 845- 862. doi: 10. 1007/ s11046- 023- 00743- z. Epub 2023 Jun 9. PMID: 37294505; PMCID: PMC- 10687130.
- Ruiz-Sánchez D, Calderón-Romero L, Sánchez-Vega JT, Tay J. Intestinal candidiasis. A clinical report and comments about this opportunistic pathology. Mycopathologia. 2002; 156 (1): 9- 11. doi: 10. 1023/ a/ 102132- 6713470. PMID: 12715941.
- Kumamoto CA. Inflammation and gastrointestinal Candida colonization. Curr Opin Microbiol. 2011 Aug; 14 (4) 386- 91. doi: 10. 1016/ j. mib. 2011. 07. 015. Epub 2011 Jul 28. PMID: 21802979; PMCID: PMC- 3163673.
- Oyom AP, Okello E, Acam V, Aramo C, Mwambi B, Okiria JC, Oyet C. Prevalence and antifungal susceptibility of gastrointestinal candidiasis among diabetic patients: A cross-sectional study. Afr J Lab Med. 2020 Dec 10; 9 (1): 997. doi: 10. 4102/ ajlm. v9i1. 997. PMID: 333- 54526; PMCID: PMC- 7736660.
- Lacour M, Zunder T, Huber R, Sander A, Daschner F, Frank U. The pathogenetic significance of intestinal Candida colonization–a systematic review from an interdisciplinary and environmental medical point of view. Int J Hyg Environ Health. 2002 May; 205 (4): 257- 168. doi: 10. 1078/ 1438- 4639- 00159. PMID: 1206- 8745.
- Otasevic S, Momcilovic S, Petrovic M, Radulovic O, Stojanovic NM, Arsic Arsenijevic V. The dietary modification and treatment of intestinal Candida overgrowth – a pilot study. J Mycol Med. 2018 Dec; 28 (4): 623- 627. Doi: 10. 1016/ j. mycmed. 2018. 08. 002. Epub 2018 Aug 27. PMID: 30166063.
- Jawhara S. Healthy Diet and Lifestyle Improve the Gut Microbiota and Help Combat Fungal Infection. Microorganisms. 2023 Jun 11; 11 (6): 1556. doi: 10. 3390/ microorganisms- 11061556. PMID: 37375058; PMCID: PMC- 10302699.
- Murugesh J, Annigeri RG, Mangala GK, Mythily PH, Chandrakala J. Evaluation of the antifungal efficacy of different concentrations of Curcuma longa on Candida albicans: An in vitro study. J Oral Maxillofac Pathol. 2019 May- Aug; 23 (2): 305. doi: 10. 4103/ jomfp. JOMFP- 200- 18. PMID: 31516248; PMCID: PMC- 6714268.
- Soliman S, Alnajdy D, El-Keblawy AA, Mosa KA, Khoder G, Noreddin AM. Plants’ Natural Products as Alternative Promising Anti-Candida Drugs. Pharmacogn Rev. 2017 Jul- Dec; 11 (22): 104- 122. doi: 10. 4103/ phrev. Prev- 8- 17. PMID: 28989245; PMCID: PMC- 5628516.
- Erdoğan, Aşkın. (2015). Small Intestinal Fungal Overgrowth. Current Gastroenterology Reports. 17. 436. 10. 1007/ s11894- 015- 0436- 2.
- Erdogan A, Rao SS. Small intestinal fungal overgrowth. Curr Gastroenterol Rep. 2015 Apr; 17 (4): 16. Doi: 10. 1007/ s11894- 015- 0436- 2. PMID: 2578- 6900.
Seek Expert Advice
Are you still struggling with persistent bloating, gas, indigestion, white-coated tongue, or fatigue even after undergoing treatment for a long time? These could be signs of a fungal overgrowth in your gut which needs deep-root treatment. At IAFA Ayurveda, under the guidance of Dr. Sahil Gupta and his expert team, we offer a complete Ayurvedic approach that targets the root cause of intestinal candidiasis.
Why Choose IAFA Ayurveda?
Personalized diagnosis based on Dosha imbalance, Agni status, and Ama formation, along with personalized treatment like detox therapy, use of herbal formulation, personalized dietary and lifestyle counseling, yoga and Pranayama for gut-brain healing, etc.
Don’t wait to make your diseases more chronic. Book a Consultation at IAFA Ayurveda today and get your personalized treatment plan to treat intestinal candidiasis naturally!
Was this Page Helpful?
So, IAFA’s Root-Cause Treatment for Intestinal Candidiasis is Just 3 Steps Away!

01. Connect With Us
Share your history of illness or Book your appointment

02. Consult With Us
Dr. Gupta a certified Ayurvedic Allergist Consultant

03. Root Cause Treatment
Get an accurate diagnosis, medicines, diet & lifestyle change
Real Case Studies – Successfully Treated Patients
Real Case Studies of Successfully Treated Patients from All Around the World by IAFA Ayurveda®
-

32-Year-Old Female Patient Recovered from Chronic Urticaria and Leaky Gut Syndrome – A Case Study
This case study highlights the successful Ayurvedic treatment of chronic urticaria associated…
-

5-Year-Old Shih Apso Dog Recovered from Canine Peripheral Neuropathy – A Case Study
This case study presents a 5-year-old Shih Tzu-Lhasa Apso crossbreed dog (pet)…
-

9 Year Old Female Patient Recovered from Chronic Allergic Bronchitis – A Case Study
This case study presents a 9-year-old female patient who has successfully recovered…
-
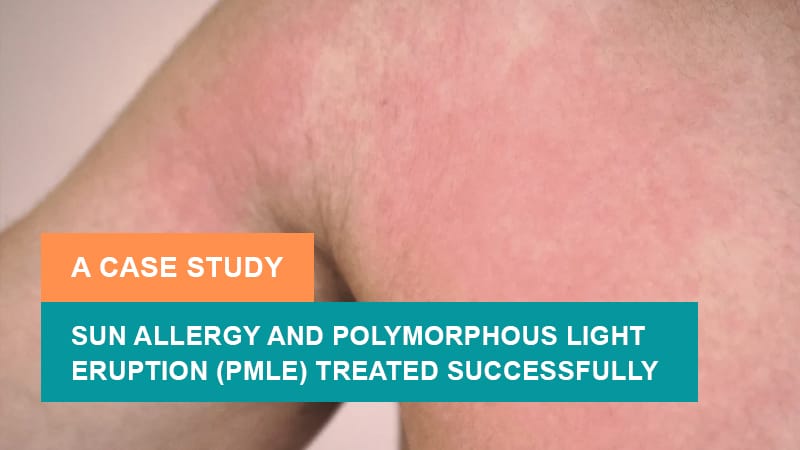
12-Year-Old Child Recovered from Solar Urticaria (Chronic Sun-Sensitivity) – A Sun Allergy Case Study
This is a case study of a 12-year-old child who has successfully…
Read More Articles
-

Polymorphous Light Eruption (PMLE)
Discover Ayurvedic treatment for Polymorphous Light Eruption (PMLE). Learn about its causes,…
-

Mast Cell Diseases
Discover Ayurvedic treatment for Mast Cell Diseases, including types, causes, symptoms, and…
-

High Immunoglobulin-E (IgE) Levels
Discover Ayurvedic treatment for high Immunoglobulin-E (IgE) levels. Learn about the causes,…








