Abstract
Background:
Dyshidrotic eczema, also known as pompholyx, is a chronic inflammatory skin condition characterized by vesicular eruptions, intense pruritus, scaling, and painful fissures primarily over the palms and soles. It often follows a recurrent course, associated with multiple triggers including allergens, stress, and infections.
In modern dermatological treatments, topical corticosteroids, immunomodulators, antifungal agents, etc., are used, yet many patients with chronic presentations face unsatisfactory outcomes, including frequent relapses of the condition. From an Ayurvedic viewpoint, such conditions can be correlated under the diagnosis of Vicharchika.
This disease is primarily attributed to an imbalance and vitiation of Kapha and Pitta doshas along with Rakta Dhatu (blood) involvement, resulting in symptoms like Kandu (itching), Sphota (blisters), Shithilata (loss of skin integrity), and Daurgandhya (foul odor). When left unchecked, this may progress to chronicity with secondary infections, including fungal colonization of nails (Dadru or Dushta Vrana) that can be considered as onychomycosis.
Case Presentation:
A 40-year-old woman with a more than two-year history of bilateral palmar or plantar dyshidrotic eczema and coexisting onychomycosis was treated with a structured integrative Ayurvedic protocol at IAFA for one and a half years, with monthly follow-up and stepwise adjustments as per condition.
Material and Methods:
The patient underwent a comprehensive Ayurvedic treatment protocol at IAFA comprising the use of internal medications, i.e., herbal juices (Swarasa), tablets (Vati), and decoctions (Kwath) targeting detoxification, dosha balancing, and Rejuvenation therapy (Rasayana) alongside external therapies (Bahaya Chikitsa) including topical application of herbal oils (Taila) and cleansing bars. Monthly clinical assessments of patients are done with modifications in treatment over one and a half years, as per the condition.
Results:
Significant improvement was observed from the second month, with progressive reduction in itching, scaling, and fissuring. By six months, palmar lesions healed substantially, and nail texture began improving.
At the final follow-up, there was no active eczema or cracks, and the nails regained normal appearance, with minimal post-inflammatory hyperpigmentation remaining.
Conclusion:
This case highlights the potential of Ayurvedic treatment to achieve sustained remission in dyshidrotic eczema with onychomycosis by addressing systemic and local factors. Regular monitoring and personalized adjustments remain crucial for long-term success.
Keywords:
Dyshidrotic eczema, Pompholyx, Vicharchika, Onychomycosis, Dadru, Dushta Vrana, Chronic eczema, IAFA
1. Introduction
Dyshidrotic eczema, also known as palmoplantar pompholyx, is a condition characterized by pruritic vesicles on palms and soles, often evolving into fissures, scaling, and secondary infection. Its etiology is multifactorial, i.e., idiopathic, due to contact allergens, sweat, stress, fungal association, etc., and it typically exhibits a chronic or relapsing course.
Modern dermatological treatment often starts with the use of topical corticosteroids, cold compresses, and emollients; refractory cases may require systemic immunomodulators, phototherapy, or biologics. Despite therapeutic advances like JAK inhibitors, IL-4, or IL-13 inhibitors for chronic hand eczema, many patients relapse after cessation of therapy.
In Ayurveda, such skin issues correspond to Vicharchika (Kustha Roga), and fungal nail involvement is seen under Dadru or Dushta Vrana. Pathogenesis involves doshas aggravation producing Ama (toxins) and Srotorodha (channel blockages), leading to local inflammation and impaired skin barrier function. When left unchecked, this may progress to chronicity with secondary infections, including fungal colonization of nails (Dadru or Dushta Vrana).
The Ayurvedic approach for such conditions is detoxification (Shodhana), dosha correction, particularly Kapha and Pitta, along with Rakta, and the use of Rasayana, along with careful dietary and lifestyle regulation. Herbal formulations with antifungal, anti-inflammatory, and immunomodulatory properties are selected carefully to restore Agni (digestive fire) and normalize doshas function.
External applications using medicated oils and herbal pastes aid in healing, pain relief, and prevention of relapses. Additionally, strict Pathya (dietary and lifestyle) management to avoid known aggravators such as wheat, dairy, and processed foods is integral to the holistic Ayurvedic therapeutic approach. This case report provides a month-by-month clinical trajectory of integrative Ayurvedic therapy in a severe, multi-year instance of dyshidrotic eczema with onychomycosis.
2. Case Presentation
A 40-year-old female from Haryana, India, presented on 14 May 2022 with a year-long history of episodic, worsening eczema involving both palms and soles. The lesions included fissures, bleeding, scaling, severe itch, and deep, painful cracks. Simultaneously, she had long-standing nail dystrophy suggestive of onychomycosis, which had been refractory to prior antifungal therapies.
Her symptoms significantly interfered with daily functions involving her hands and walking. Her diet history revealed frequent consumption of wheat or gluten, dairy, processed foods, etc. There was no significant or known allergy history. On general examination, she had hyperemic, scaly, fissured skin over palms and soles, and her nails were thickened, brittle, discolored, and deformed.
The initial Ayurvedic assessment diagnosed Vicharchika predominantly Kapha–Pitta and Rakta Dushti, coupled with Dadru or Dushta Vrana of the nails. The therapeutic aim was root-level correction by internal or external repair, and strict Pathya Ahara-Vihara discipline.
2.1 Patient Details:
- Age/Sex: 40/F
- Address: Haryana, India
- Duration of Illness: More than 2 years
2.2 Chief Complaints:
Bilateral palmar and plantar cracks, deep sores, flaking, bleeding, severe itching, eczematous rashes, and chronic fungal nail infection interfering with daily life.
2.3 Diagnosis:
- Modern: Dyshidrotic eczema with onychomycosis
- Ayurveda: Vicharchika with Dadru or Dushta Vrana of nails (Nakha)
2.4 Triggers and Exacerbating Factors:
Wheat or gluten, dairy, processed foods, and frequent dietary indiscretion.
3. Methods
3.1 Intervention Protocol:
This work is reported as a single-patient, longitudinal case study with structured monthly follow-up over 16 months, i.e., from 14 May 2022 to 9 September 2023. The patient was treated and monitored at the Institute of Applied Food Allergy (IAFA), Gohana, Haryana, India. Clinical documentation, photographs, and prescriptions were recorded at each visit.
The Patient received Ayurvedic treatment, including topical agents like IAFA E-5 Cell Repair Oil, AF-7 Cream, Skin Fresh Bar, and oral formulations like Bhoomi Amla Swaras, Shirish Swaras, Makoye Swaras, Mahamanjishthadi Kashayam, etc., along with a strict gluten- and dairy-free diet and lifestyle modifications.
Monitoring: Structured monthly follow-up visits, i.e., from 14 May 2022 to 9 September 2023, with clinical assessment, photographic documentation, and progressive adjustment of prescriptions.
3.2 Ayurvedic Treatment Protocol:
External: IAFA E-5 Cell Repair Oil, AF-7 Cream, IAFA Skin Fresh Bar, all with standardized usage protocols for hands, feet, and nails.
Internal: Formulation or single drugs like Bhoomi Amla Swaras, Shirish Swaras, Makoye Swaras, Changeri Capsules, Haridrakhandham Choornam, Pitpapara Capsules, Triphala, Maha Manjishthadi Kashayam, Satyanashi Swaras, Praval Panchamrit Mouktik, AF-7 Tea, etc.
Diet or Lifestyle: A Diet free from gluten, dairy, packaged foods, and the use of fresh, home-cooked meals, seasonal vegetables and fruits, herbal teas, etc.
3.3 Table of Ayurvedic Treatment Protocol for different follow-ups
| Category | Follow-up Date | Medicines given internally or externally | Purpose |
| Initiation phase | 14 May 2022 | Internal: Bhoomi Amla Swaras, Aahar Amrutham Rasa, Skin Detox tablets, Anthram Mithram Gulika, Triphala capsules. External: IAFA E-5 Cell Repair Oil, AF-7 Cream, IAFA Skin Fresh Bar. | Detoxification of Rakta and Pitta reduces inflammation, itching, and oozing, and begins skin and nail repair. |
| Early Follow-up | 14 Jun 2022 | Bhoomi Amla Swaras, Aahar Amrutham, Skin Detox Tablet, Anthram Mithram Gulika, Triphala; E-5 Cell Repair oil, AF-7 Cream, Skin Fresh Bar. | Monitor early response and maintain barrier repair and detox. |
| Early Balancing Phase | 16 Jul 2022 | Shirish Swaras, Changeri Capsules, Haridrakhandham Choornam, Kutaj Ghan Vati, Aahar Amrutham Rasa, Anthra Mithram Gulika, in addition to ongoing topicals. | Correct Kapha-Pitta imbalance, improve gut digestion, reduce persistent inflammation. |
| Mineral and Immunomodulatory Support | 16 Aug 2022 | Mouktik Pishthi, Aam Visha Balance Tab, Changeri Capsules, Haridrakhandham Choornam, Aahar Amrutham Ras, Shirish Swarasa, in addition to ongoing topicals. | Immunomodulation strengthens the skin barrier and reduces Ama (metabolic toxins). |
| Digestive Support | 22 Oct 2022 | Triphala Swaras is newly added with Bhoomi Amla Swaras, Aahar Amrutham Rasa, Changeri Capsules, Haridrakhandham Choornam, and Anthra Mithram Gulika in addition to ongoing topicals. | Bowel regulation and continued prevention of toxin (Ama) re-accumulation. |
| Anti-inflammatory and Blood Purification | 06 Dec 2022 | Makoye Swaras, Punarnava Swaras, Bhumi Amalaki Swarasa with Pitpapara capsules, AF-7 Tea, Anthram Mithram Gulika, in addition to ongoing topicals | Deep detox, anti-inflammatory effect, liver and kidney support for persistent plantar or nail involvement. |
| Mineral Support | 25 Jan 2023 | Same Swarasa previously prescribed with Praval Panchamrit Mouktik Yukt Tablet, Skin Detox Tablet, AF-7 tea, Pitpapra capsules, in addition to ongoing topicals. | Mineral (Rasayana) support, enhanced immunity, wound healing, and strengthening. |
| Skin Rasayana | 11 Mar 2023 | Same Swarasa use along with Mahamanjishthadi Kashayam, Parval Panchamrit Mouktik Yukt tablets in addition to ongoing topicals. | Broad dosha balancing, blood purification, promotes skin regeneration and pigmentation correction. |
| Relapse Control and Antimicrobial Boost | 22 Apr 2023 | Satyanashi Swaras, Bhoomi Amalaki Swarasa with skin detox tablet and AF- 7 tea, with existing external medicines. | Target recurrent itching or lesions with stronger antimicrobial and antifungal support. |
| Recovery Phase | 22 Jun 2023 | External local application continued along with Bhoomi Amalaki Swarasa, skin detox tablet, and AF-7 tea. | Prepare for gradual tapering and maintenance. |
| Maintenance therapy for 1 month | 09 Sep 2023 | Continue external care as needed, E-5 Cell Repair oil, AF-7 Skin Fresh Bar. Internal medication Bhoomi Amalaki Swarasa, Satyanashi swarasa, Skin Detox Tablet, AF-7 tea, Pravala Panchamrit Mouktik Yukt Tablets, and long-term diet rules. | Prevention of recurrence through maintenance therapy and diet rules. |
4. Result
4.1 Before and During Treatment Images
Deep cracks and sores over palms and soles, with flaky skin. Eczematous rashes over the body and fungal infection in the nails of the hands and feet.

4.2 Monthly Follow-Up Clinical Status
| Date | Clinical Status and Progress |
| 14-May-2022 | Initiation. Severe palmar or plantar eczema, nail onychomycosis, extreme pruritus, and cracks. |
| 14-Jun-2022 | Approximately 20% symptom relief. Itching over flexors. |
| 16-Jul-2022 | Same relief and symptoms maintained. |
| 16-Aug-2022 | Persistent cracks and sores, no new worsening. |
| 22-Oct-2022 | Hands recovered from the patches and itching shifted to the lower limbs. |
| 06-Dec-2022 | Approximately 50% reduction in itching, hands clear, feet and nails not fully resolved. |
| 25-Jan-2023 | Approximately 70% less itching, and the hands are clear. |
| 11-Mar-2023 | Approximately 70% less itching, and the hands are clear. |
| 22-Apr-2023 | Relapses of itching in the lower and upper limbs despite healed hands. |
| 22-Jun-2023 | Approximately 90% symptom relief in cracks, sores, and itching on the feet. |
| 09-Sep-2023 | Hyperpigmentation remains post-inflammatory, no itching, cracks, or sores, palms, soles, and nails are fully healed. |
4.3 After Treatment Images
Palms, soles, and nails have returned to normal. No scaling, itching, cracks, or active eczematous features are present. Nails regained strength and natural color. No limitations in activity. Only mild post-inflammatory hyperpigmentation remained, which was explained to the patient.

5. Discussion
Dyshidrotic eczema with nail involvement, i.e., onychomycosis, is a chronic, relapsing condition that often returns even after modern treatment. Modern treatment, such as steroids, antifungal drugs, and topical creams, may provide temporary relief, but they are associated with side effects, drug resistance, and incomplete results.
In this case, an Ayurvedic approach applied step by step over 16 months led to long-term remission in a patient with a two-year history of severe, non-responsive disease.
The month-by-month follow-up showed how digestive correction, Dosha-balancing formulations, Rasayana therapy, and external local care gradually restore skin and nail health. Early improvement of approximately 20% by June 2022 was achieved with Bhoomi Amla Swaras, Skin detox tablet, Anthram Mithram Gulika, and Triphala capsules, which reduced inflammation, regulated digestion, and supported immunity.
By December 2022, the introduction of Makoye Swaras, Punarnava, and Pitpapara enhanced blood purification (Rakta Shodhana) and reduced itching and swelling, resulting in approximately 60–70% improvement. By mid-2023, deeper Rasayana medicines such as Mahamanjishthadi Kashayam and Praval Panchamrit Mouktik promoted skin regeneration, improved pigmentation, and strengthened overall immunity.
At the last follow-up in September 2023, the patient had complete remission with no itching, fissures, or nail deformities. The therapeutic effect can be explained by the known actions of the formulations. Haridrakhandham is recognized for its anti-inflammatory properties. Kutaj Ghan Vati supports gut health and immunity, and Mahamanjishthadi Kashayam acts as a blood purifier and improves complexion.
In the same way, other formulations exhibit anti-microbial effects, promote skin regeneration, etc. Along with this, there is mineral support that strengthens newly repaired tissue and speeds healthy nails and skin restoration. The combined use of internal and external treatments, along with dietary regulation and avoidance of triggers such as gluten, dairy, and processed foods, reflects the Ayurvedic principle of helping to treat both root cause and Dosha imbalance. Major strengths of this case are regular monitoring and Ayurvedic formulation adjustment at each stage, which ensured steady progress and likely prevented relapse.
At the same time, certain limitations must be acknowledged. Being a single case, the results cannot be generalized. Fungal clearance was not confirmed with laboratory tests, which would have strengthened the scientific validity. Despite these limitations, the case provides meaningful evidence that an Ayurvedic treatment protocol can achieve long-term remission in chronic skin and nail disorders.
6. Conclusion
This single case study demonstrates that Ayurvedic treatment protocols like blood purification, Rasayana support, healthy gut support, and external applications can achieve remission in chronic dyshidrotic eczema with nail involvement.
Stepwise therapy and regular follow-up played a key role in ensuring steady improvement and preventing relapse. The patient not only recovered but also maintained remission if followed dietary rules (Pathya and Apathya), which is rarely observed with conventional therapies.
Although limited to a single case, these findings highlight the potential of Ayurveda as a safe and effective approach for managing chronic, treatment-resistant skin and nail disorders.
7. Clinical Significance
This case study highlights that individualized Ayurvedic therapy, with proper follow-up and lifestyle guidance, can provide long-term remission in chronic dyshidrotic eczema and onychomycosis. Such outcomes suggest Ayurveda may serve as a valuable approach where modern treatments show limited success.
Happy Review from the Patient
The patient visited along with her spouse and expressed her gratitude towards IAFA Ayurveda® and Dr. Sahil Gupta for excellent results she had got with Ayurvedic treatment of Dyshidrotic Eczema and Onychomycosis. The team IAFA Ayurveda® felt happy as another success story has been added into our books. You can read the wonderful comments we received from our patient. We feel grateful to become a part of their health journey and provide them a better life.
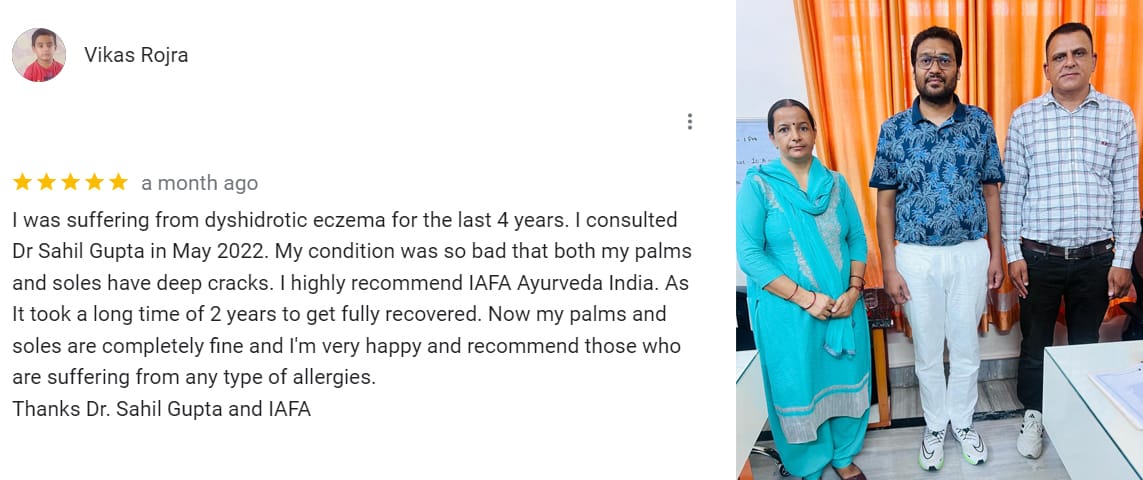
Reference:- https://g.co/kgs/47Dnby4
Dr. Sahil Gupta Final Note
This case study presents a remarkable Dyshidrotic Eczema Recovery Journey and Onychomycosis Healing Process in a patient who had suffered from chronic symptoms for more than two years.
Through step-by-step Ayurvedic treatment, including blood purification (Rakta Shodhana), Rasayana support, and strict lifestyle management etc., the patient experienced a full transformation, moving from painful cracks and brittle nails to complete recovery.
Led by Dr. Sahil Gupta and his expert team at IAFA, this Pompholyx Eczema Case Study highlights how integrative Ayurvedic treatment can deliver lasting remission, where modern therapies often fail to provide satisfying results. This report further contributes to classical Ayurvedic literature, showcasing a modern example of the Vicharchika Case Study, Dyshidrotic Eczema Patient Success Story, and Dushta Vrana Case Study.
Such Chronic Eczema Patient Recovery journeys and Holistic Healing Case Studies inspire hope for those struggling with long-standing conditions, and Ayurveda’s role as a safe, effective, and sustainable healing path.
If you are going through similar problems like eczema, onychomycosis, allergies, or chronic skin conditions, we invite you to consult Dr. Sahil Gupta for various allergy and skin care solutions.

References
- Agnivesha, Charaka, Dridhabala. In: Charaka Samhita, ed. Vaidya Jadavaji Trikamji Aacharya, editor. Varanasi: Chaukhamba Sanskrit Sansthan; 2009.
- Shinde, Dattatraya & Patil, Vishakha. (2022). A Conceptual Review of Vicharchika with Special Reference to Eczema. 10. 2455- 6211.rid of allergies. Be ready to improve your life and make it healthier because we are ready to heal you and be a part of your health journey!
- Sushruta. In: Sushruta Samhita, Sutra Sthana, ed. Vaidya Jadavji Trikamji Acharya, editor. Varanasi: Choukhambha Orientalia; 2005.
- Vagbhata. In: Ashtanga Hrudaya, 9th ed. Anna Moreshwar Kunte, Krishnashastri Navarre, Harishastri, editors. Varanasi: Choukhambha Orientalia; 2005.
- Bhavamishra. In: Bhava Prakasha Nighantu 11th ed., part 2. Brahma Shankara Mishra, editor. Varanasi: Choukhambha Bharati Academy; 2009.
- Dr. Gyanendra Pandey, Dravyaguna Vigyana, reprint 2012, Chawkhamba Krishnadas Academy.
- Calle Sarmiento PM, Chango Azanza JJ. Dyshidrotic Eczema: A Common Cause of Palmar Dermatitis. Cureus. 2020 Oct 7; 12 (10): e10839. doi: 10. 7759/ cureus.10839. PMID: 3317- 3645; PMCID: PMC- 7647- 841.
- Abreu-Velez AM, Pinto FJ Jr, Howard MS. Dyshidrotic eczema: relevance to the immune response in situ. N Am J Med Sci. 2009 Aug;1 (3): 117- 120. PMID: 2266- 6682; PMCID: PMC- 3364640.
- Venkatesh S, Fakhraie S, Chovatiya R. Recalcitrant Dyshidrotic Eczema Successfully Treated with Upadacitinib. Dermatitis. 2023 Nov-Dec; 34 (6): 569- 570. doi: 10. 1089/ derm. 2022. 0070. Epub 2023 Mar 28. PMID: 3697- 6810; PMCID: PMC- 1053- 3710.
- Kiszla BM, Orlowski TJ, Kole LCS. Efficacy and tolerance of upadacitinib in the treatment of dyshidrotic eczema. JAAD Case Rep. 2023 Jun 25; 38: 141-143. doi: 10. 1016/ j. jdcr. 2023. 06. 024. PMID: 3752- 1189; PMCID: PMC- 1038- 2852.
- Vocks E, PlOtz SG, Ring J. The Dyshidrotic Eczema Area and Severity Index – A score developed for the assessment of dyshidrotic eczema. Dermatology. 1999; 198 (3): 265- 9. doi: 10. 1159/ 0000- 18127. PMID: 1039- 3450.
- Ikumi K, Kio T, Torii K, Masuda H, Morita A. Successful treatment of dyshidrotic palmoplantar eczema with ultraviolet A1 light-emitting diodes. J Dermatol. 2020 Aug; 47 (8): 922- 923. doi: 10. 1111/ 1346- 8138. 15402. Epub 2020 May 22. PMID: 3244- 1347; PMCID: PMC- 7497185.
- Li Y, Xiao J, Sun Y, Fang H, Qiao J. Quick Treatment of Very Severe Refractory Hand and Foot Eczema with Dupilumab: A Case Report and Literature Review. J Asthma Allergy. 2023 Jan 5; 16: 1- 8. doi: 10. 2147/ JAA. S399340. PMID: 3663- 6704; PMCID: PMC- 9830185.
- Li Y, Xiao J, Sun Y, Fang H, Qiao J. Quick Treatment of Very Severe Refractory Hand and Foot Eczema with Dupilumab: A Case Report and Literature Review. J Asthma Allergy. 2023 Jan 5; 16: 1- 8. doi: 10. 2147/ JAA. S399340. PMID: 3663- 6704; PMCID: PMC- 9830185.
- Arya TU, Rao US; From the proceedings of Insight Ayurveda 2013, Coimbatore. 24th and 25th May 2013. PA03.01. A clinical study on the management of vicharchika (eczema) by Brihat Haridrakhanda and lepa of arka taila in children. Anc Sci Life. 2013 Jan; 32 (Suppl 2): S70. Doi: 10. 4103/ 0257- 7941.1238- 93. PMCID: PMC- 4147544.
- Kaur M, Chandola HM. Role of rasayana in the cure and prevention of recurrence of vicharchika (eczema). Ayu. 2010 Jan; 31 (1): 33- 9. doi: 10. 4103/ 0974- 8520. 68207. PMID: 2213- 1682; PMCID: PMC- 3215- 319.
- Hegde P, Hemanth DT, Emmi SV, Shilpa MP, Shindhe PS, Santosh YM. A case discussion on eczema. Int J Ayurveda Res. 2010 Oct; 1 (4): 268- 70. Doi: 10. 4103/ 0974- 7788.76792. PMID: 2145- 5456; PMCID: PMC- 305- 9451.
- Salethoor SN, Kulangara S, Aramya AR, Puthiyedath R. Ayurvedic management of a refractory skin disease clinically diagnosed as Cutaneous Lichen Planus-A case report. J Ayurveda Integr Med. 2024 Mar-Apr; 15 (2): 100884. Doi: 10. 1016/ j. Jaim. 2023. 100884. Epub 2024 Mar 20. PMID: 3851- 3503; PMCID: PMC- 1097- 2801.
- Yousefian F, Smythe C, Han H, Elewski BE, Nestor M. Treatment Options for Onychomycosis: Efficacy, Side Effects, Adherence, Financial Considerations, and Ethics. J Clin Aesthet Dermatol. 2024 Mar;17 (3): 24-33. PMID: 3849- 5549; PMCID: PMC- 10941855.
- Elewski BE. Onychomycosis: pathogenesis, diagnosis, and management. Clin Microbiol Rev. 1998 Jul; 11 (3): 415- 29. doi: 10. 1128/ CMR. 11. 3. 415. PMID: 966- 5975; PMCID: PMC- 88888.
- Chetana K, Menon R, David BG, Ramya MR. Clinicomycological and Histopathological Profile of Onychomycosis: A Cross-sectional Study from South India. Indian J Dermatol. 2019 Jul- Aug; 64 (4): 272- 276. doi: 10. 4103/ ijd. IJD- 160- 18. PMID: 3151- 6135; PMCID: PMC- 6714189.
- Jazdarehee A, Malekafzali L, Lee J, Lewis R, Mukovozov I. Transmission of Onychomycosis and Dermatophytosis between Household Members: A Scoping Review. J Fungi (Basel). 2022 Jan 6; 8 (1): 60. doi: 10. 3390/ jof- 8010060. PMID: 3505- 0000; PMCID: PMC- 87794- 52.








